In an interview with PatientsEngage, Dr Dorairaj Prabhakaran, Vice President – Research and Policy, PHFI and one of the main authors of the study answers questions on the findngs and implications of population based study on Hypertension in India.
The Silent Killer or Hypertension continues to strike us with an estimated 10.8% of all deaths, which equates to 9.4 million deaths each year worldwide1. These are the statistics from the study published by Nature’s Journal of Human Hypertension. A second population based study2 by the Public Health Foundation of India (PHFI), Harvard T.H. Chan School of Public Health, Heidelberg Institute of Global Health, University of Birmingham and University of Gottingen, shows that although the prevalence of hypertension is high in India, the awareness and treatment of the condition is low. The findings of the study are summarized below:
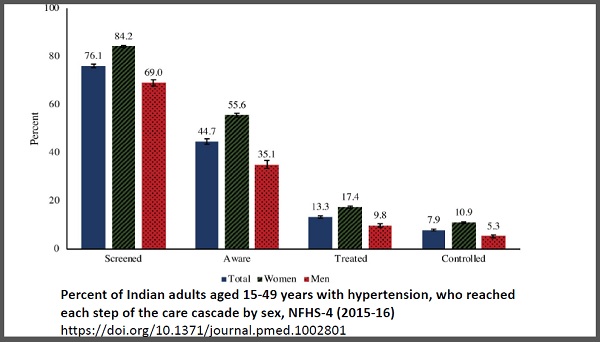
- 3 out of 4 individuals with hypertension had ever had their blood pressure measured.
- Less than half of individuals (45%) had been diagnosed.
- Less than 1 in 7 (13%) reported currently taking hypertensive medication.
- Less than 1 in 10 (8%) had their blood pressure under control.
- Adults living in rural areas, men, and those who were poorer, were even less likely to receive the care they need.
- Only 5.3% of hypertensive men and 10.9% of hypertensive women aged 15-49 years have their blood pressure under control (i.e. they are taking medications and have a normal blood pressure).
- There is huge state-level variation in hypertension screening. Screening of hypertensive individuals was lowest in Madhya Pradesh (61.3%) and highest in Haryana (93.5%).
- More than half of Indians aged 15-49 years with hypertension are not aware of their hypertension status. Awareness level was lowest in Chhattisgarh (22.1%) and highest in Puducherry (80.5%).
- 27 major states/union territories have blood pressure control rates below 10%. Daman and Diu was the highest, but still only 1 in 5 adults there are under control.
Dr Dorairaj Prabhakaran, Vice President, Research and Policy, at PHFI and one of the lead authors of the studies said “Detection of hypertension is straightforward, treatments are simple yet effective, and hence hypertension can be easily controlled. Control of hypertension prevents future stroke, heart attacks and deaths. However, it is an unfortunate paradox that India does not perform well in any of the measures of detection, treatment and control. I believe the new National Health Mission through the health and wellness clinics has the potential to address the issue.”
In an interview with PatientsEngage Dr Dorairaj Prabhakaran, sheds more light into the studies and helps us understand the importance of correct diagnosis of hypertension.
1) Your study states that there was a 63% higher prevalence of hypertension diagnosis when only the first reading was considered in comparison to the average of the second and third readings. What are your recommended guidelines for Hypertension diagnosis?
Our recommended guidelines for the number of Blood Pressure (BP) measurements to arrive at final clinic is to take the average of the second and third BP readings. This is what is recommended by the ESC/ESH 2018 guidelines as well. However, considering that reclassification in optimal, normal and high normal categories is minimal and plays a less significant role in deciding the final management plan, in limited resources settings as that seen in India, we would recommend repeated BP measurements only in individuals with an initial BP reading in grade 1 (>140/90 mmHg) or higher categories of BP.
2) In what ways, can a standard protocol be implemented by all medical professionals/centers through the country?
Standardized training of all healthcare professionals in proper BP measurement technique is critical. Training should be part of the undergraduate and postgraduate teaching curriculum for medical students. Physicians that have completed training must be sensitized through continuing medical education programs. Considering the increasing burden of hypertension, the shortage of medical practitioners and the involvement of allied healthcare professionals, it is important to ensure adequate training of all those involved in BP screening including Accredited Social Health Activists and Auxiliary Nurse Midwifes that are part of the National Health Mission initiative of universal screening of hypertension, diabetes and three common cancers.
3) What are the hazards of wrong diagnosis?
Improper measurement and interpretation of office BP can lead to overestimation of a patient’s true BP and inaccurate classification, which in turn exposes the patient to unnecessary treatment and its associated adverse effects. When considered at a population level it can lead to overestimation of the prevalence of hypertension in a population, influence inappropriate health policy decisions and lead to a waste of limited national resources.
4) If incorrectly diagnosed, what are the side-effects of hypertensive drugs that can be harmful to the patient i.e. unwanted complications of hypertensive drug use in normal persons?
Treatment of any medical illness with drugs entails the risk of unwanted adverse effects. The risk of side effects of antihypertensive medication is the same for a normal and hypertensive patient. However, the exposure of these normal individuals to the risk of side effects is unnecessary and should be avoided.
5) What are the factors that can cause variation in BP?
The accuracy and interpretation of a BP measurement is dependent on individual level factors, the device being used and the observer, of which the observer is often described as the most fallible component. In 1964, Geoffrey Rose and his colleagues classified observer error into three categories - systematic error, terminal digit preference and observer prejudice or bias. Although most of these observer-level errors can be avoided by replacing manual devices with automated ones, the highly labile nature of BP in itself can affect the accuracy and reliability of a measurement. The observer should be aware of the considerable variability that may occur in BP from moment to moment with respiration, emotion, exercise, meals, tobacco, alcohol, temperature, bladder distension and pain. Hence in clinic settings it is advisable to take BP after the patient has rested for some time, not had coffee or smoked one hour prior to the measurement. Ambient room temperature should be comfortable and the BP should be measured in a seated and relaxed position.
6) How is White-coat hypertension detected?
Anxiety increases BP by as much as 30 mmHg or more and may be regarded as a physiological reaction. This is not substantially influenced by reassurance and familiarization. Out-of-office measurements help diagnose white coat hypertension (labelling normotensives as hypertensives). Out-of-office measurements include home BP monitoring and ambulatory BP monitoring.
7) Are there any protocols for diagnosing low blood pressure?
Low blood pressure is not a clinical entity and does not require treatment if the patient does not have symptoms. It is usually found in sick hospitalized patients where appropriate treatment should be initiated. Sometimes patients who are started in antihypertensive treatment complain of giddiness particularly after getting up from a seated position. This may be related to postural fall in BP which can be corrected by reducing/altering the anti-hypertensive medication.

References:
- Impact of repeated blood pressure measurement on blood pressure categorization in a population-based study from India. Dorairaj Prabhakaran et al. Journal of Human Hypertension (April 2019).
- Hypertension screening, awareness, treatment, and control in India: A nationally representative cross-sectional study among individuals aged 15 to 49 years. Jonas Prenissl, Dorairaj Prabhakaran et al. PLOS Medicine ( May 2019).