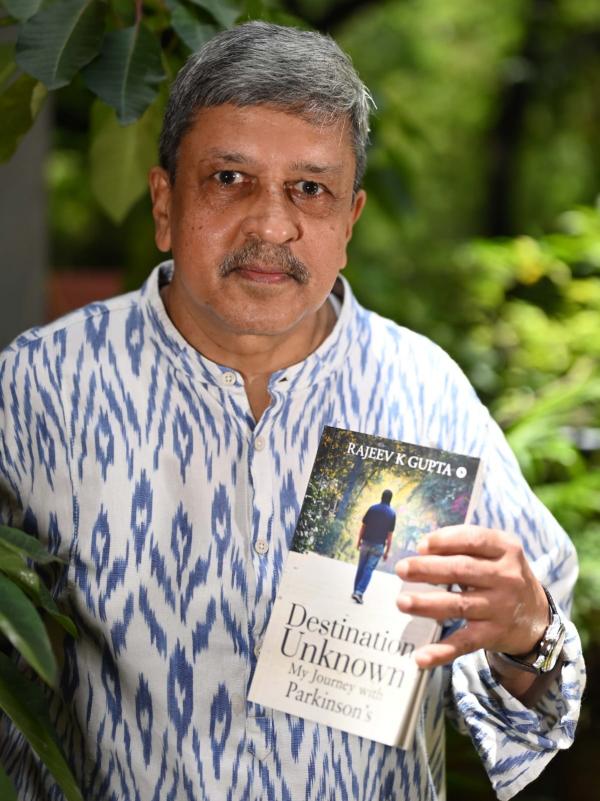
Rajeev K Gupta, who lives with Parkinson’s, recounts his own experiences with many surprising and not so well-known non-motor symptoms of PD like sleep behaviour disorders which can be a nightmare and others like facial masking, speech problems, drooling which can be quite discomforting and distressful. This article is reviewed by Neurologist Dr. Prashanth LK.
Most people know Parkinson’s Disease (PD) as a disease with shaking hands or tremors. You may be surprised to learn that tremors are not the defining symptom of the disease. A person with Parkinson’s (PWP) may not experience tremors during the entire course of the disease. Slowness of movements and limbs, medically known as bradykinesia, is experienced by most patients right from the early stages of the disease. Hence, if we insist to name a primary symptom of PD, it would be bradykinesia and not tremors.
Movement disorders or movement related symptoms (gait, posture, balance, fine motor functions etc.) are visible and are easily identified specially in communities with a PD patient among them. Parkinson’s presents many more not so well-known symptoms that may be quite discomforting if not outright debilitating. Some of these symptoms may be very embarrassing for PWPs, so much so that many PWPs stop socializing and go into a shell thus further complicating their condition.
I am describing here some of these lesser-known PD symptoms. I have personally experienced these symptoms to various degree and in various stages of the disease during my ten years of living with Parkinson’s.
Sleep Disorders
One fine night in mid-January this year, I found myself kneeling on the floor, elbows on the bed and face in my palms, musing about life at 3:00 a.m. in the morning. I noticed a pool of blood gushing from my mouth on the white bed sheet. My first thought was that our bedsheet and mattress were getting soiled. It took me some time to realize that one of my teeth was broken and two others badly shaken, threatening to come out any time.
I tried to recollect the sequence of events and how I ended up on the floor. I remembered seeing a vivid dream. I was standing in front of a tea kiosk in a remote area waiting for my cuppa. The kiosk was adjacent to a huge boundary wall and a crowd there was looking at something. Being curious, I joined them too. There was a crack in the wall and a yellow snake was stuck in the crack struggling to come out. With one final effort, the snake broke free and darted towards me (Meee!! Of all the people in the crowd, sigh!). I jumped up to avoid the snake. In reality, I leapt out of the bed falling 2-3 feet away from the edge, my upper teeth hitting the far-end corner of the bedside table.
This was not the first time I enacted my dream. A few weeks back, I was fighting and kicking a guy in my dream and ended up hitting my wife Renu, sleeping next to me, hard on her shin. She got up screaming….and while I was busy pleading innocence, she quietly picked up her bed and baggage and moved to a spare bedroom in the house.
When I discussed this with my neurologist, he informed me that this is known as RBD (REM Sleep Behaviour Disorder), a common sleep disorder in PD along with insomnia and vivid dreams. In RBD, a person acts out his or her dreams. Because these dreams often involve being chased or attacked, people will yell, punch, kick or even leap out of bed.
REM is the period of sleep during which we dream. Normally, the brain inhibits muscle movement during this time. In RBD, the brain pathways that suppress muscle activity are disrupted, and people are able to move to act out their dreams.
I was surprised to know that this is a treatable symptom, yet many patients/families do not inform the doctor.
And we thought that Parkinson’s is all about tremors and gait!
Facial Masking
Medically known as hypomimia, facial masking makes a person’s face blank or expressionless. Like the muscles involved in movements, other muscles such as face muscles slow down too, making it difficult and slower for a PWP to make simple facial gestures such as smiling and raising an eyebrow. These symptoms creep in slowly as the disease progresses.
Facial and body expressions play a major role in inter-personal communication. Hence, a PWP with hypomimia, may be easily mistaken as indifferent or disinterested even when she is trying her best to be friendly. PWPs are also more likely to be disbelieved as their expressions are not matching their statements. For example, I may be truly saying that I am enjoying life and feeling happy but since my expressions are not corroborating my statement, my friends and family may take it as an attempt to hide my sadness.
If friends and family are not sensitized and are not sensitive to this, this may lead to avoidable misunderstandings and may affect one’s relationships.
Speech Problems
Almost 75% to 90% of PWPS develop voice and speech difficulties (dysarthria) over the course of their illness.
The most common speech problems experienced by people with PD involve reduced volume, reduced pitch range or monotone, and difficulty with the articulation of sounds. In essence, you can’t speak as loudly as others, you find it more difficult to convey emotion when you do speak, and you find it difficult to form the words you are trying to pronounce. Speaking clearly and intelligibly becomes difficult.
If you have Parkinson’s disease (PD), you probably notice that people often ask you to repeat what you just said. It may be tempting to withdraw from conversations with others altogether, but that would be a mistake. You need to interact with others on a daily basis, no matter how frustrating it becomes — this is critical for your mental health, and be assured that your loved ones want to interact with you.
Simple voice exercises like – joining laughing clubs, blowing a conch, practicing breathing exercises, practicing speaking loud and slowly, may help to manage this.
Swallowing
Difficulty swallowing, called dysphagia, can happen at any stage of Parkinson’s disease. It usually starts mildly with issues such as taking a longer time to eat a meal or coughing at mealtimes. It can progress over time to become a critical PD symptom.
Signs and symptoms vary from mild to severe. In the beginning it may just be difficulty swallowing certain foods or liquids, coughing or throat clearing during or after eating/drinking and feeling as if food is getting stuck.
As the disease progresses, swallowing can become severely compromised and food/liquid can get into the lungs, causing aspiration (when food or liquid “goes down the wrong pipe”).
In severe cases, this may lead to aspiration pneumonia. Aspiration pneumonia is the leading cause of death in PD.
Drooling
Excessive drooling, medically known as sialorrhea, is a common symptom of Parkinson’s. It may start with mild wetting of the pillow while sleeping or little drippings when sipping liquid from a cup or a glass. In advanced stages, this may result in continuous dribbling of saliva during unguarded moments. This may get very embarrassing and may lead to awkward social situations.
In PD, the amount of saliva that the body produces is normal or in some cases, less than the normal. But swallowing issues – swallowing less often or not completely – lead to saliva pooling in the mouth.
The average person swallows about 1,000 times a day. And for most of us we do not even know we are doing this. Drooling in Parkinson’s occurs when there is excessive saliva in the mouth which leaks out because people with Parkinson’s may subconsciously not be swallowing frequently enough.
Interestingly, drooling, along with face-masking, speech and swallowing difficulties, is included among non-motor symptoms even though the root cause is motor: decreased coordination, slowness of movement (bradykinesia) and rigidity of the muscles of the mouth and throat.
Depression
Most of the PWPs deal with depression during some stage of the disease (in some cases even before the PD Diagnosis.) Depression in PD may not be a persistent symptom. It may come and go.
Though managing the challenges of living with Parkinson’s is depressing enough, it is not the only cause of depression in PWPs. Chemical changes in the brain caused by the pathology of the disease are the main factor. Thus, we can say that in PD, depression is caused by one or more of the following factors:
- Biological Factor- chemical changes in the brain caused by the disease itself e.g., dopamine deficiency.
- Psychological Factor – emotional reaction to PD diagnosis and living with the challenges thrown by PD.
- Side effects of PD medications
Maintaining a physically and mentally active life, socializing, meditation etc. are some of the natural ways to manage depression. It is important to keep your doctor informed of any drastic changes in your general mood or daily routine. If necessary, and if prescribed by your doctor, do not hesitate to take medicines to overcome your blues.
This is not an exhaustive list. There are many more symptoms associated with PD such as fatigue, muscle cramps, urinary problems, smell loss, orthostatic hypotension etc. (Please refer the picture for a complete list of symptoms) I have elaborated here only some of the symptoms that, in my view, make most social impact making it necessary to make communities, including friends and families of PWPs, aware of these symptoms.
The good news is that most of these symptoms can be managed well through early recognition and proper treatment through occupational therapies and medications. Awareness and acceptance are the keys.
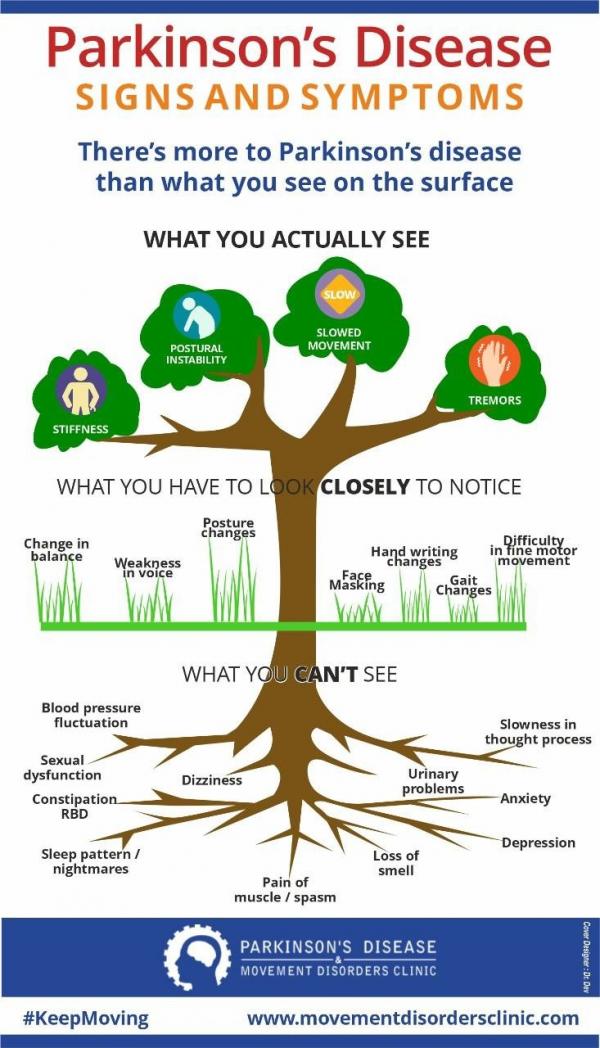
This image has been kindly contributed by Parkinson's Disease and Movement disorders clinic and the design has been created by Dr. Dev and Dr. Prashanth LK.
References:
https://www.parkinson.org
https://www.parkinson.org.uk
https://www.parkinsonsresource.org
https://www.michaeljfox.org
https://www.movementdisordersclinic.com
This article is a patient viewpoint and not a medical opinion.
(The writer is a PD patient and author of the book Destination Unknown – My Journey with Parkinson’s)