Dr Shital Patel answers all that you want to know about oral contraceptives, how they work, when you should use them, side effects, do they increase the risk of cancer?
What are Oral Contraceptives?
Oral contraceptives are hormonal preparations that may contain progesterone or combination of oestrogen and progestin. The combination drug prevents pregnancy by inhibiting the release of the hormones - luteinizing hormone (LH) and follicle stimulating hormone (FSH) from the pituitary gland in the brain. LH and FSH are important in the production of the egg and preparing the uterus lining for implantation of the embryo.
Progestin hinders the sperm from penetrating and, therefore, fertilising the egg.
There are three types of combination pills available:
1. Monophasic birth control pills deliver the same amount of oestrogen and progestin every day.
2. Biphasic birth control pills deliver the same amount of oestrogen every day for the first 21 days of the cycle. During the first half of the cycle, the progestin/estrogen ratio is lower to allow the lining of the uterus (endometrium) to thicken as it normally does during the menstrual cycle. During the second half of the cycle, the progestin/estrogen ratio is higher to allow the normal shedding of the lining of the uterus to occur.
3. Triphasic birth control pills have constant or changing oestrogen concentrations and varying progestin concentrations throughout the cycle. There is no evidence that bi- or triphasic oral contraceptives are safer or superior to monophasic oral contraceptives, or vice versa, in their effectiveness for the prevention of pregnancy.
How and when to take the pills?
Usually, birth control pills are packaged either as 21 or 28 day units. In the 21-day package, a pill is to be taken daily for 21 days followed by a 7 day gap. For the 28-day units, the pill is taken for 21 days, followed by a 7 day period during which a placebo pill(containing no medication) is taken. Newer formulations are now available with 24 (hormone) + 4 (placebo) pills, continuous or extended regimens, in which only the active hormone pill is taken.
For the first seven days of starting the pill, additional contraception must be used because pregnancy may occur during this period [Just to be extra safe and give the pill time to kick in.] Failure to take the pill can result in pregnancy! If a pill is forgotten, it should be taken as soon as possible. If more than one pill has been missed, instructions on the packaging should be followed or your local doctor should be consulted.
Can birth control pills be used to delay a period?
Yes, birth control pills can be used to reduce or eliminate a period. If you are on the 21 day pack, simply skipping the placebo pills and starting right away on a new pack will omit your periods. There are several birth control pill regimens that prevent bleeding for three months or an entire year. This works best when taking a monophasic pill where the same hormone dose is taken.
How soon after stopping the birth control pill can one conceive?
Once the pill is stopped, periods should return in 4-6 weeks time and ovulation will resume. One can get pregnant at anytime after that.
What if periods don’t resume after stopping the pill?
When periods don’t resume for several months after the pills have stopped, you may have a condition called Post-pill Amenorrhea. In some women, the menstrual cycle fails to regulate after the birth control has stopped. Your gynecologist must be informed of this immediately.
Can I take a pregnancy test while being on the pill?
Pregnancy tests are designed to test a hormone called human chorionic gonadotropin (HCG), which is produced by the uterus after implantation. The birth control pills do not affect the level of HCG and hence you can get accurate results from a pregnancy test while you're on the pill.
What are the effects of taking the pill accidently while being pregnant?
This is a very common accident and rarely does it harm the baby. However, once the pregnancy has been detected, the pills must be stopped immediately.
What are emergency contraception pills?
Emergency Contraception pills are used when a woman has had unprotected sex. This pill is commonly called the "morning-after pill”. This pill should be taken within 72 hours of having sex and is more effective when taken within the first 24 hours. It contains levonorgestrel and is available over-the-counter at drugstores, as well as health clinics and Planned Parenthood. (Levonorgestrel works by delaying or preventing ovulation and even stopping the sperm from fertilizing the egg.) Brand names include Plan B One-Step, Next Choice to name a few. Ulipristal acetate (Ella) also is approved for emergency contraception but is only available by prescription.
Related reading: Frequently Asked Questions on Emergency Contraception Pills
Can you stop birth control pills at any time or do you have to finish the current packet?
Yes the pill can be stopped at any time. It’s always best to inform your OBGYN and discuss other forms of birth control once the pill has stopped.
Can you get pregnant during the week that you take the placebo pills?
If the pills are taken regularly, the placebo does not increase chances of pregnancy. Birth control pills are considered 99% effective in preventing pregnancies. If a pill has been missed, the risk increases. Hence a condom should be used as back-up contraception.
Do birth control pills increase the risk of cancer?
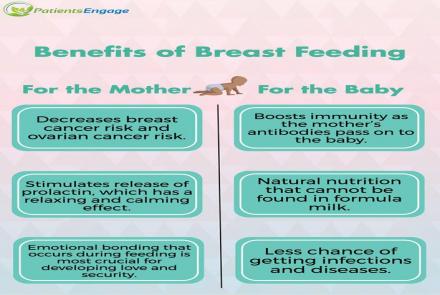
Oral contraceptives are known to reduce the risk of ovarian and endometrial cancer. This protective effect increases with prolonged use of oral contraceptives pills. Birth control pills are associated with an increased risk of cervical cancer. This may be largely due to the fact that sexually active women have a higher chance of becoming infected with human papillomavirus (HPV), which causes virtually all cervical cancers.
According to the National Cancer Institute, the risk of breast cancer, especially among younger women does increase a little with the use of oral contraceptives. We are not sure by what percentage it raises risk. This risk, however, returns to normal 10 or more years after discontinuing use.
Research Update Jan 2018 on the increase in risk of breast cancer due to hormonal birth control pills:
Experts point out that the overall risk was miniscule with only 1 extra case of breast cancer among 7,700 women using such contraceptives per year. There is good data to show that five or more years of oral contraceptive use substantially reduces ovarian cancer and endometrial cancer risk. So women should evaluate the results against the benefits of the pill for other cancers.
There is also an increased risk of getting benign liver tumours, but the relationship between oral contraceptive use and malignant liver tumors is less clear.
Do birth control pills affect cholesterol levels?
There are different kinds of birth control pills that affect cholesterol. Some are combination pills, with oestrogen and progestin, while others are "mini-pills" with just progestin. Oestrogen may affect triglyceride levels and total cholesterol levels causing HDL (the "good" cholesterol) to increase and the LDL ("bad" cholesterol) to decrease.
Progestin does the opposite and causes decrease in HDL and an increase in LDL.
However, these changes in blood levels are not strong enough to have any significant effect.
Do birth control pills affect blood pressure?
Birth control pills may slightly increase blood pressure. This risk is higher in women who smoke, are overweight and have a family history of heart diseases. Doctors do regularly check blood pressure in all women on pills. If you already have high blood pressure, your doctor will discuss other forms of birth control.
Can women above 35 years of age continue taking birth control pills?
Oral contraceptives are usually not recommended to women above 35, because of increasing risk of developing heart disease. Birth control pills may slightly affect cholesterol levels, raise blood pressure, worsen glucose tolerance and increase the risk of rare blood clots. If a woman has any heart disease risk factors, the pill is not recommended after 35, but if a woman is healthy, new studies show that it is okay to continue the pill till early 50s. The final call lies with the doctor and patient and continued monitoring of the cardiovascular system.
Can antibiotics interfere with the birth control pills?
Antibiotics usually do not affect birth control pills and their actions except for Rifampin. Studies clearly show that Rifampin decreases the effectiveness of birth control pills in preventing ovulation. However, Rifampin is not commonly prescribed today.
What are the side- effects of oral contraceptive pills?
Most side-effects are only temporary and subside in a few months. Most common side effects include headache, breast tenderness, nausea, weight gain, irregular bleeding, and mood swings.
There may be an increase in migraine frequency especially in women with a history of migraines. Conversely, women whose migraines are triggered by hormone fluctuations may notice improvement in their migraines.
Unusually, oral contraceptives may contribute to increased blood pressure, blood clots, heart attack and stroke. Women who smoke, are over the age of 35, and have a history of blood clots or breast or endometrial cancer, are advised against taking oral contraceptives, as these conditions can increase the adverse risks of taking oral contraceptives.