People with Parkinson's are at high risk of falling due to problems with balance, rigidity, and slowness of movement. Here we bring key safety strategies to reduce incidence of falls that can cause bumps, bruises or even broken bones.
Some people with Parkinson’s find their pattern of walking (gait) changes; you may walk more slowly, shuffle, or you may experience freezing of gait when you stop and are unable to move for a few seconds or minutes. These changes in walking pattern can affect your balance and make falls more likely, particularly as Parkinson’s progresses.
But not everyone with Parkinson’s is susceptible to falls, although statistically people with Parkinson's are more likely to fall over than people without. Falls tend to happen most when movement changes suddenly, for example when you turn around, or when you do more than one thing at a time, such as carrying an item whilst walking.
Falls tends to be forwards, and occasionally sideways, and can lead to bruises, cuts, or even fractures and broken bones, so it is important to be aware of the likely causes of falls and understand how to minimise the risks.
People with and without Parkinson’s may be more susceptible to falls if they have limited movement, are old or frail, have dementia or depression or if they take medications that cause drowsiness.
What causes falls in Parkinson’s?
Poor balance (postural instability) and freezing are probably the most common causes but there may be many contributing factors.
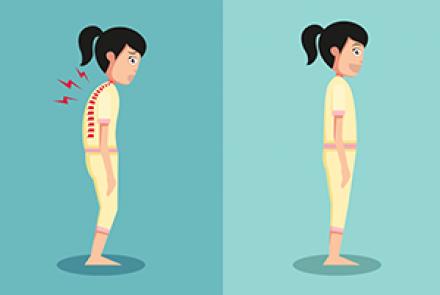
- Stooped posture - the stooped posture that often occurs as Parkinson’s progresses increases the risk of falling forwards.
- Postural instability - because Parkinson’s affects the area of the brain (the basal ganglia and brainstem) that controls walking and plays an important part in adjusting balance as you move, you may not have the normal reflexes to quickly adjust position and save yourself from falling, or to maintain balance when you shift your weight. For example, you may be unable to put your arms out to balance yourself when walking on an uneven surface or unable take an additional short step to avoid falling when tripping.
- Reduced muscle tone - muscle weakness may make posture more stooped (bent forwards) which also increases the risk of falling. If is therefore important to stay as active as possible so as to prevent muscle weakening and to stop joints from getting weak or stiff.
- Freezing of gait – freezing - when you involuntarily suddenly stop walking or are unable to initiate a movement as your feet feel ‘glued’ to the floor - may last just a few seconds or for several minutes. This can make you feel unsteady and therefore more likely to fall. See also Freezing.
- Low blood pressure (orthostatic or postural hypotension) - when we move from lying or sitting to standing up our blood vessels should automatically adjust to keep our blood pressure even. But sometimes this does not happen - perhaps as a result of dehydration, illness or medication side effects – and we feel light-headed as blood flow to the brain is reduced. This can lead to fainting and falls. So it is important to get up slowly – and don’t try to start walking immediately - and be aware that there is an increased risk of falls when you get up. Blood pressure problems can be a side effect of Parkinson’s medications. Other drugs, such as those used to treat high blood pressure, can also increase dizziness on standing. Make sure you discuss any faintness you feel with your doctor as your medication may need to be adjusted.
- Eyesight – in some people Parkinson’s can cause eye problems such as blurred vision or difficulty judging spaces. This can make it more difficult to safely move past objects or through narrow spaces and so the risk of falling is increased. It is important to discuss any eye problems with your doctor as these could be a side effect of medication. Always have regular eye check-ups so that your vision is as clear as possible.
- Hazards in your home or at work - many falls can be avoided with careful planning and organisation. Even the smallest hazard, like laundry left on the floor, can lead to a fall and injury. Falls are more likely to occur if you experience incontinence and have to rush to the bathroom, particularly during the night. An occupational therapist will be able to advise on ways to reduce risks in your home or at work.
Reducing the risk of falls
It is important that you take all your Parkinson’s medications as prescribed so that symptoms such as poor gait and freezing are well controlled.
Some Parkinson’s medications may, unintentionally, lower blood pressure and this can cause dizziness and increase the risk of falling. If this happens you should ask your doctor or nurse to check your blood pressure both when standing and sitting. Your doctor may be able to advise on medication to help with low blood pressure and dizziness, although this can be complicated because of possible interference with Parkinson’s medications.
Some dizziness can be avoided. For example, when getting out of bed let your feet dangle over the side of the bed for a few minutes before standing and then rise slowly. When getting up from a chair, pause for a few moments and only start walking when you feel steady.
Some Parkinson’s medications can actually aggravate falls by causing dyskinesias (impairment of voluntary movement) and freezing. Again, it is important to tell your doctor if you fall so that medication can be adjusted if necessary.
Caution!
You are more likely to fracture a bone if you fall frequently, particularly if you have osteoporosis. If you fall frequently, ask your doctor for an osteoporosis assessment. If osteoporosis is diagnosed, he or she will be able to give you advice on minimising its effects or refer you to another professional who can help.
If you have recently had a fall then, statistically, you are much more likely to have another within the next six months. So it is important that you tell your doctor and carer if you fall so that you can together do all you can to prevent falls.
Who can help?
There are a lot of things you can do to help yourself but there are also experienced professionals who can provide useful advice. Depending on where you live, your doctor may be your first contact and they may refer you to another expert. In some countries a Parkinson’s Disease Nurse Specialist or nurse who specialises in neurology will also be able to advise.
Physiotherapists
A physiotherapist will address specific problems related to:
- posture
- gait (and freezing of gait)
- balance and falls
- transfers (ie moving from a chair or bed)
- reaching and grasping.
He or she will be able to suggest an exercise programme and teach you different movement strategies to make everyday tasks as easy and safe as possible. Exercises are very important in preventing or reducing muscle stiffness, which will in turn reduce the risks of instability and falling. Good posture is important in keeping your balance and you may be advised on exercises to help with maintaining or improving your physical fitness and posture.
A physiotherapist can also advise your carer and suggest appropriate ways of helping you to move, for example getting out of bed safely. If you fall frequently, a physiotherapist can teach you different ways to get yourself up and moving again, and help restore your confidence.
An occupational therapist will be able to help you maintain as much independence as possible in your everyday life. He or she will be able to assess your home and daily routine then suggest ways of making activities as safe and as manageable as possible. Often very simple adjustments to the set-up of your kitchen or bathroom, for example, can make a big difference to your mobility, quality of life and risk of falling. They can also advise on practical aids, equipment or adaptations that might help you, as well as suggestions to improve your ability to carry out specific tasks such as dressing or cooking.
Podiatrists
A podiatrist (also known as a chiropodist) will be able to advise if you have a foot problem that may be causing you to fall. He or she will also be able to suggest the most suitable types of footwear to prevent falls.
(This information about falls was generously supplied by the European Parkinson's Disease Association)