Says Dr V Shanta, cancer specialist and the Chairperson of Adyar Cancer Institute, Chennai. Lung cancer, which is related to smoking, is today the top cancer in the country. Within the year, 15.5% of 13 to 15-year-olds are going to start smoking. Don’t let your child be one of them. Plus, how smoking harms non-smokers, too.
1. How grave is the health problem posed by tobacco use in India? How much of it relates to smoking cigarettes, beedis and how much is it due to consumption of gutka, paan masala, paan?
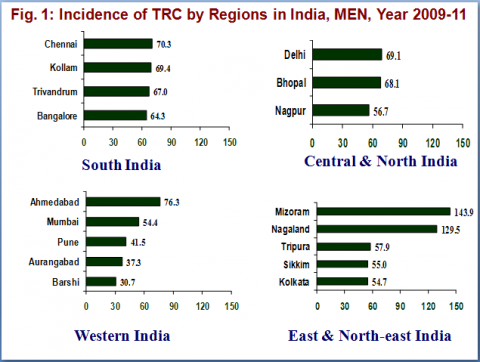
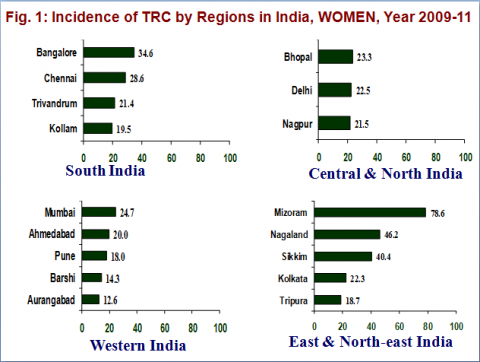
The magnitude of the problem of cancer in India is in a large way related to tobacco in some form. 40% of cancers in men and 20% of cancers in women are tobacco related. There is a general rise in tobacco habit in different areas of India. One of the highest are the north eastern states. In Tamil Nadu tobacco-related cancers (TRC) in the female is going down and this is related to educational level.
Beedi is the most popular tobacco product used and constitutes 48% of the tobacco market, chewing tobacco 38% and cigarettes 14%.
According to me, tobacco control is cancer control and cancer control is tobacco control.
2. Has there been any shift in tobacco use, behaviour over the last few decades? Is the generation who are now in their 30s or 40s smoking less? Are there fewer cases of tobacco-related cancers among them? And how is the younger generation doing?
According to global adult Tobacco survey, 34.6% of adults use tobacco in some form
Youth 14.6% use tobacco in some form
4.4% smoke cigarettes
12.5% use other tobacco products
As per Global Youth Tobacco Survey
15.5% of never smokers are likely to initiate smoking soon. There is no reduction in adult tobacco habits in India. Tobacco related cancers have gone down among women who are essentially tobacco chewers.
Important:
Tobacco related cancers are on the rise in men. Lung cancer, which occupied the 4th or 5th rank among cancers in men in 1984-85, today is the leading cancer among men occupying the top rank and related to tobacco smoking.
Tobacco habit – essentially smoking, has been documented as going down in the US and UK, from 40-59% adult habit, it is now down to 20%.
In addition, lung cancer incidence and mortality have come down significantly in the US and UK.
3. How is India doing in its fight against tobacco use? What needs to be done? What has been the failure of the public education programmes?
India signed the Framework Convention on Tobacco Control (FCTC) on February 5, 2004. Cigarettes and other tobacco control act is enacted, major provisions are ban on smoking in public places, prohibition of sale to minors, ban on sale around educational institutions and ban on promotion and advertisement. However, enforcement continues to be the challenge. Although FCTC has provided guidelines, not much is being done on supply side measures, such as providing alternative livelihood to tobacco workers, farmers, bidi rollers.
Interdepartmental co-ordination is lacking. In the new proposed amendments, it is recommended to set up a National Tobacco Control Organization. This should be done immediately to enhance the co-ordination among different departments and to have a common vision in terms of tobacco control.
What has been the failure of the public education programmes?
FCTC urges all the countries to make financial arrangements within the country to ensure the sustainability of the efforts. Despite the magnitude of the problem, there is no single dedicated individual in any of the Governments for tobacco control. Integrating tobacco control into every health care programme is essential to reach the maximum.
Tobacco board needs to be closed or its role needs to be revised to encourage the tobacco farmers and industry to other crops/business. Political will is still lacking for tobacco control. Tobacco industry needs to be made accountable for the damages.
(Provided by Dr. Vidhubala, Head of Anti-Tobacco Activity)
4 You have said that schools should not hire smokers as teachers. What else can schools do to steer kids away from smoking?
What can families do? What should you say to youngsters who think smoking is cool?
The target population for anti-tobacco education has to be the youth – 10 to 14 years.
Parents at home and teachers in school should be role models. This can change the tobacco habit scenario.
Tobacco control has to have an integrated educational programme; dealing with “habits” both as a health hazards and as a “bad habit” (way of life).
When we were children anybody using tobacco or alcohol was taboo.
There was a stigma attached to them. Today it is the reverse. It is a fashion.
Declining values and principles in life is thus a major factor and should be reversed.
Tobacco habit is higher among children whose parents/teachers are tobacco users.
Similarly, hostels or the work place where there are more smokers, encourages the start of addiction.
Younger Generation
Newer forms of tobacco are marketed by the industries to attract youth and children including chewing tobacco. Few statistics are given below.
According to the Global Youth Tobacco Survey (13 to 15 years) conducted in India in 2009:
14.6% currently use any tobacco product (Boy = 19.0%, Girl = 8.3%)
4.4% currently smoke cigarettes (Boy = 5.8%, Girl = 2.4%)
12.5% currently use other tobacco products (Boy = 16.2%, Girl = 7.2%)
15.5% of never smokers are likely to initiate smoking next year
Second hand smoke exposure (Passive Smoking): 21.9% live in homes where others smoke in their presence and 36.6% are bystanders and are around others who smoke in places outside their home.
Cessation
66.1% want to stop smoking
67.2% tried to stop
The fact is that once the habit is formed, the quit rate is very low – less than 12%.
That is why I say that tobacco habit is a disease and as in all disease, prevention is better than cure.
The parent in the home and teacher in the school thus play a vital role and must understand their responsibility.
Cancer Institute (WIA) study showed that in Chennai, 10-13-year-old students, 3.2% were using tobacco and want to continue tobacco use.
Exposure to smoking at home – passive smoking is reported as 39.5%.
Students who buy tobacco products for their parent is 28.6%. This is dangerous.
Education in general about hazards of tobacco should identify all major illnesses like cancer, cardiovascular disease, cerebro vascular disease, chronic pulmonary obstructive disease and many others as major factors in these illnesses.
Tobacco is not only a causative factor in the disease but increase the mortality rate in disease like tuberculosis, diabetes etc.
5. What is the incidence of survival in tobacco related cancer patients?
We cannot club all tobacco related cancers together. It will depend on the site of cancer, can be oral cancer, oropharyngeal cancer, larynx, lung etc. Pattern of survival varies from site to site, patient to patient, agewise, comorbid conditions and most importantly stage of disease.
Early cancer is curable. A tobacco habitue if he continues to use tobacco even during treatment of his cancer has distinctly a poorer chance of curability – as reported by the Surgeon General Report from US.
The message that needs to be dinned into the public mind is:
- Prevent cancer by not using tobacco
- Early cancer is curable.
- If one continues to use tobacco when he or she is under treatment, the outlook is poorer.
6. I read that children whose parent smoked are at risk of cancer even if they do not smoke themselves. Is this correct and if so, how common is this
Yes, passive smoking is documented as a factor in increasing the risk of cancer in women and children. We do not have reliable data in India but there are few in the US.
Meta analysis revealed 20% to 2-fold excess risks of lung cancer among life-long non-smokers whose spouses were smoking compared to non-smoking spouse with direct relationship to frequency of smoking and duration of marriage. The excess risk of lung cancer in non-smokers exposed to second-hand smoke in childhood varied between 20% to >2-fold (this is not statistically significant). An excess risk of 80-90% was observed for colo-rectal cancers among non-smoking subjects exposed to second-hand smoke in Sweden. A positive trend in excess risk of gastric cardia cancer associated with lifetime exposure to second-hand smoke was observed among never-smoked men in Canada. (Gastric cardia cancer affects the top of the stomach near the junction of the oesophagus.)
Meta analysis revealed excess risk of coronary (or ischaemic) heart disease in never smokers exposed to second-hand smoke between 6-78% (a major risk factor for heart disease).
Children are at excess risk of cancer with exposure to parental smoking.
In 1986, the first review of evidences declared that cancers of the lung, oral cavity, pharynx, larynx, oesophagus, pancreas, urinary bladder and renal pelvis are related to tobacco use in some form.
In the Indian context, only cancer of the cervix can be excluded from this list of tobacco related cancers as prevalence of tobacco smoking among women is negligible.
In the Indian context, the male preponderance observed in TRC incidence is more attributable to tobacco smoking while most cancers among women were attributable to tobacco chewing.
There is sufficient evidence in humans for the carcinogenicity of smokeless tobacco. Smokeless tobacco causes cancers of the oral cavity, oesophagus and pancreas.
Read Dr. Shanta's interview on socio economic centricity here: http://www.patientsengage.com/news-and-views/significant-number-cancer-…;