From popping pills for Parkinson's Disease every 2 hours and dealing with various side effects of these pills, Hari has turned his life around and chose to focus on his passions for travel and spreading awareness on PD. Read on.
I was diagnosed with Parkinson's Disease in 2008. Currently after the Deep Brain Stimulation surgery, I seem to have recovered almost 95%. Earlier I used to pop pills every two hours. My consumption of medicines has now come down to at the most one per day.
What…

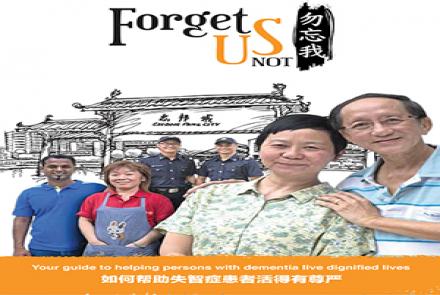
Sometimes the Daily activties like Bathing, Dressing and Eating can be a huge challenge for caregivers looking after a person with dementia. Here are a few useful tips. Let us know which one you find helpful.
Tips for Bathing
For some people bath time can be a frightening, confusing experience.
- Plan the bath or shower for the time of day when the person is most calm and agreeable. Be consistent. Try to develop a routine.
- Tell the person what you are going to do, step by step, and allow him/her to do as much as possible.
- Prepare in advance. Make sure you have everything you need ready and in the bathroom before beginning. Draw the bath ahead of time.
- Be sensitive to the temperature. Warm up the room beforehand if necessary and keep extra towels and a robe nearby. Test the water temperature before beginning the bath or shower.
- Minimize safety risks by using a handheld showerhead, shower bench, grab bars, and non-skid bath mats. Never leave the person alone in the bath or shower.
- Bathing may not be necessary every day. A sponge bath can be effective between baths.
Tips for Dressing
Getting dressed could present a series of challenges: choosing what to wear, getting some clothes off and other clothes on, and struggling with buttons and zippers.
- Try to have the person get dressed at the same time each day so he/she will come to expect it as part of the daily routine.
- Encourage the person to dress himself/herself to whatever degree possible. Plan to allow extra time so there is no pressure or rush.
- Allow the person to choose from a limited selection of outfits.
- Arrange the clothes in the order they are to be put on to help the person move through the process with ease.
- If the person needs prompting, provide clear, step-by-step instructions.
- Choose clothing that is comfortable, easy to get on and off, and easy to care for. Elastic waists and Velcro enclosures minimize struggles with buttons and zippers.
Tips for Eating
- Ensure a quiet, calm atmosphere for eating. Limiting noise and other distractions may help the person focus on the meal.
- Provide a limited number of choices of food and serve small portions. You may want to offer several small meals throughout the day in place of three larger ones.
- Use straws or cups with lids to make drinking easier.
- Substitute finger foods if the person struggles with utensils. Using a bowl instead of a plate also may help.
- Have healthy snacks on hand. To encourage eating, keep the snacks where they can be seen.
- Visit the dentist regularly to keep mouth and teeth healthy.
Coming up next week : Tips on staying active & alternate therapies !
Condition