- With inputs from Dr. Anju Virmani, Endocrinologist, New Delhi
What is it
People with diabetes, due to high blood glucose, often have a loss of fluid in the body. This can cause dry skin on the legs, elbows, feet and other areas of the body. Dry skin is more likely to crack, allowing germs to get into these areas, causing infections that can have severe consequences. Diabetics are more prone to getting bacterial and fungal infections.
Diabetics may also suffer from itchy skin due to the lack of circulation. Scratching the skin also lays it open to the possibility of infection.
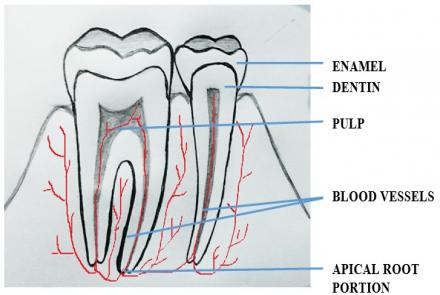
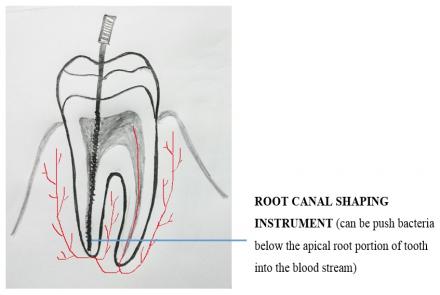
Diabetes Mellitus also brings about changes to the blood vessels, which can cause skin complications. Also, in longstanding diabetes, nerve damage may occur. The deadened nerves may not send information about injury or infection to the brain, so that you may, for instance, have a blister on the foot that you are unaware of, leading to complications.
Are you at risk
Diabetics are at higher risk of developing skin conditions. People with uncontrolled diabetes may take longer to clear up the infections.
Can these skin conditions be prevented
Keeping blood sugar under control is the best preventive measure. It is also important to keep your skin in good condition with good hygiene, especially of the feet.
Keep the following in mind:
- Make sure your skin does not get too dry or cracked.
- Use gentle soaps and moisturise lightly. A very moist surface is not good either as it may encourage fungal growth.
- Use moisturisers for dry skin, and talcum powder where sweat collects, e.g. between toes and underarms.
- Clothing should be able to absorb sweat (e.g. cotton socks), and should not be too tight.
- Do not scratch your skin and treat infections and cuts immediately
- Do not walk barefoot; always wear slippers even at home or socks at places of worship like temples.
- Inspect the soles of your feet with a mirror, and between toes, carefully at least once a week, to make sure there are no undetected injury or infection sites.
Types of diabetes-specific skin conditions
Patients with Type 2 diabetes more often develop skin infections, whereas those with Type 1 more often have autoimmune-related lesions.
The following are some of the skin conditions to watch out for:
• Diabetic shin spots (also called Diabetic Dermopathy) are small brown patches on the shins of individuals with longstanding diabetes. Lesions are asymptomatic and irregularly shaped. It is the most common skin problem among diabetics. It commonly occurs in men over 50 years of age. There is no treatment; however care should be taken to avoid trauma or secondary infection. The lesions gradually resolve in 12 to 18 months. Use of bio-occlusive dressing is recommended.
• Tinea pedis or Athlete’s foot is a reddish rash usually seen between the toes. It is caused by fungal infection and is treated with standard antifungal agents. Severe cases may require Griseofulvin and the patient should be encouraged to use cotton socks.
• Onychomycosis is thickened, discoloured nails caused by fungal infection. It is treated with Griseofulvin, Itraconazole or Terbinafine hydrochloride.
• Lipohypertrophy are fatty deposits at the site of insulin shots. It can also affect insulin absorption by the skin. Ensure insulin shots are rotated within the same area daily, and if there is hypertrophy, avoid that area till the deposits clear up.
• Acanthosis nigricans is a condition in which dark, thickened skin due to hyperkeratosis appears in the body folds of the neck and armpits. It is more common in obese individuals and is a sign of insulin resistance. It is left untreated normally. It tends to diminish with reduction of insulin levels (regular exercise, reduced calorie intake, better diabetes control. Less common conditions include:
• Scleroderma like syndrome (SLS) or Waxy skin syndrome is the sclerosis or waxy thickening of the skin on hands and fingers often found in young individuals with Type 1 diabetes. Sclerosis is the tightening of the skin when it shrivels and wrinkles. SLS causes limited joint mobility as well and may be associated with microvascular complications. It’s left untreated normally but it is a warning sign to improve glucose control to prevent other complications.
• Necrobiosis lipiodica diabeticorum (NLD) appears as a reddish to brown coloured thickening of the skin, often with a rim of raised inflamed areas and central depression. This gives the skin a scaly appearance. It usually occurs on the shin and on the chest and arms. It is more prevalent in women.
The lesions may ulcerate due to trauma. It is normally left untreated unless there is ulceration. If there is ulceration, the doctor may recommend excision (removal) and skin graft.
• Xanthoma diabeticorum (Eruptive xanthoma) are small (1-3cm) yellow, raised papular skin lesions on the elbows, hips and buttocks, often itchy. These are associated with poor glycaemic control. This is treated by managing blood sugar.
• Diabetic scleroderma or scleredema: It presents with thickening of the skin on the back, shoulders and the neck that cause immobility of the tissues. It is prevalent in Type 2 diabetics. It has been reported in diabetic patients with poor metabolic control. Scleredema diabeticorum is a distinct cutaneous condition peculiar to diabetic individuals and ought not to be confused with scleroderma.
Therapeutic options are limited with generally poor results. PUVA treatment (phototherapy) and physiotherapy are therapeutic options that seem to be of some help.
• Vitiligo: Skin de-pigmentation. More common in Type 1 diabetes. A possible warning sign for polyglandular autoimmune syndrome. Avoid sun exposure, use sunscreen and cosmetic treatment if necessary.
• Lichen Planus: Flat, polygonal, erythematous lesions on the skin, white stripes with reticular pattern occurs mainly on wrists and dorsa of feet and lower legs. Treated with topical corticosteroids with or without topical cyclosporine.