
Aishwarya M, a migraineur-teacher who teaches reading and writing to middle school girls at Pune, India shares her experience of being prepared for the uncertainty of chronic migraine.
Is it possible to have a debilitating disability such as chronic migraine and still be a together teacher?
Short answer: Yes
The long answer follows.
In 2014, Maia Heyck-Merlin’s The Together Teacher: Plan Ahead, Get Organized, and Save Time! not only saved my time, it saved my life. I slowly stopped running around like a headless chicken and found my footing as a new teacher. Over the next two years, I repeatedly revised my togetherness system to almost perfect. Just when I thought I had it all conquered, life happened.
Maia says that different teachers define togetherness differently but all together teachers demonstrate the five essential skills of prioritization, planning, organization, execution and efficiency.
For me, being together is being able to organized, planned, and calm enough to be a good teacher. It may sound simple, but a lot goes into ensuring that things run smoothly in a school setting. Togetherness is one of the first things that chronic illness patients lose. They are no longer able to keep up with things, follow up and follow through. In most jobs, this can be costly. In teaching it is more so because unless you are on top of your schedule, paperwork, grading and plans, teaching is impossible.
A freak sneeze on a cold December morning in 2017 brought everything to a standstill. Something in my neck snapped and triggered the worst migraine of my life. It lasted 12 days and knocked the wind out of my sails. My doctor informed me that my episodic migraine had regressed into chronic migraine. My body slowly turned into a train wreck. I was angry, frustrated, dejected, and anxious, all at the same time. It felt like the life I had carefully orchestrated for myself was snatched away from me.
Over the next six months, I repeatedly tried and failed to bring my life back in order. My daily worksheet, weekly worksheet, and monthly comprehensive calendar – the pillars of my sanity – no longer kept me on top of things; instead they stared at me each night, reminding me of everything I could no longer do and be. Migraine had taken over my life.
The Migraine Trust reports that migraine is ranked globally as the seventh most disabling disease among all diseases. The innumerable triggers and paralyzing pain along with short term memory loss, loss of the sense of time and difficulty finding words makes living hard. A MIDAS (Migraine Disability Assessment) score of 40+ had already started sowing seeds of doubt in my mind about my ability to continue being a teacher. Being a together teacher seemed too far fetched. Thankfully, Ayurveda and my supportive husband kept me from accepting that all was lost.
Over the last 1.5 years, my MIDAS score has been consistently decreasing, and about a year ago, I began to believe that I can get my life back. I tried to get back on track using my carefully created togetherness system. It didn’t take long to realize that I couldn’t keep up. I could never go beyond 2 days on track: migraine, migraine aura or sometimes just fear kept ensuring that my system collapsed. I had to come to terms with the fact that my old ways wouldn’t work anymore and find a way to integrate my new companion, however painful, to my togetherness system. This post briefly describes the results of my experiments with making friends with pain.
1. Live in advance
It's easier to beat pain when you are ahead of pain.
I ensure that I am ahead in both my school work and house work to overcome the angst of not having assurances of future time. I plan the following week's lessons in a 4-hour time chunk on Saturdays and cook the next day's meals every evening. I have had to compromise and accept that I am not as responsive as I'd like to be in my lesson plans, and that I don't eat freshly cooked meals.
2. Buffer, and then buffer some more
It is easier to make friends with pain if you make time for pain.
I incorporate buffer time in the order of 25-50% to every task. This includes four days of housework instead of seven, and scheduled downtime on all evenings and Sundays. Large buffer times allow guilt-free suffering on migraine days while enabling rest and rejuvenation on non-migraine days. Ergo, fewer migraine days.
3. Automate pain and recovery
Pain is easier to suffer through when you know exactly what to do.
My inability to think well during a migraine often leads to poor choices and lasting regret. Here's what I use I avoid any important thinking at the time:
- A medicine kit with medicines and other migraine essentials that are easy to find even with eyes closed.
- Drafts of messages (pic below) that I can send to colleagues, friends, and family during the pain. This greatly eases my anxiety about jeopardising relationships.
- A bare minimum list (pic below) of just enough tasks to expedite recovery and prevent a giant mess that unravels once the pain subsides. The list is devoid of all tasks that can wait. It prevents me from having to prioritize tasks in the middle of agony and reduces the stress of having to find time for reset days after the postdrome.
- A first-things-first list of tasks that I need to do soon after postdrome to help me get back on track as soon as possible.
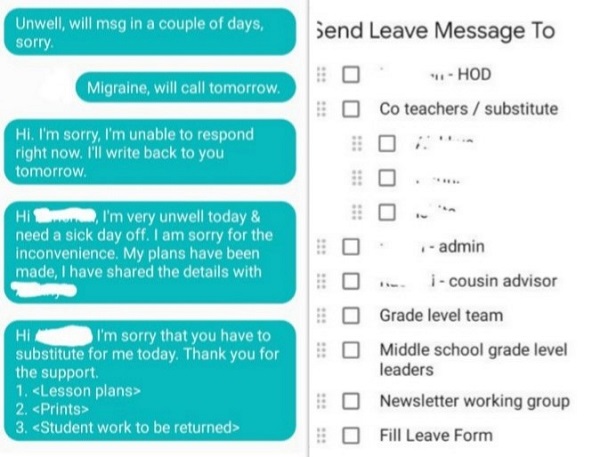
Image above: The checklists and message templates
All grand plans notwithstanding, there are days when the pain incapacitates me beyond what careful planning and preparation can salvage. There are other days when my brain is so cognitively compromised that I forget that there's a system I have built to help myself. And then, there are the plain, hopeless days when I am so depressed that I resign to fate and give up.
Although the only way out of pain, brain fog, and dejection is through them, my togetherness system slightly makes it easier for me to be patient with myself.
















