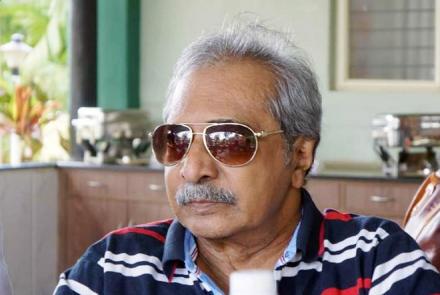
Endoscopy guru and leading gastroenterologist Dr Vipulroy Rathod’s comprehensive interview on gastrointestinal diseases and cancers makes for an enlightening and interesting read.
What is Gastroenterology?
Gastroenterology is the branch of medicine focused on the digestive system and its disorders.
Diseases affecting the gastrointestinal tract, which include the organs from mouth to anus, along the alimentary canal, are the focus of this specialty. Physicians practicing in this field are called gastroenterologists.
Which are some of the common gastrointestinal diseases?
- Acid Reflux, Heartburn, GERD
- Dyspepsia/Indigestion
- Nausea and Vomiting
- Peptic Ulcer Disease
- Abdominal Pain Syndrome
- Belching, Bloating, Flatulence
- Biliary Tract Disorders
- Gallbladder Disorders
- Gallstone Pancreatitis
- Gallstones in Women
- Constipation and Defecation Problems
- Diarrhea (acute)
- Diarrhea (chronic)
- Irritable Bowel Syndrome
- Hemorrhoids and Other Anal Disorders
- Rectal Problems in Women
Is gallstone the most common type of gall bladder disease? Are gallstones more common in females than males?
Yes, Gallstone is most common type of gall bladder disease. Gallstone disease is 2 to 3 times more common in female than male.
Read: What does Bhanu do when she got Gallstones during her pregnancy.
What is ulcerative colitis? What are its main causes?
Ulcerative colitis is a chronic disease of the large intestine, also known as the colon, in which the lining of the colon becomes inflamed and develops tiny open sores, or ulcers, that produce pus and mucous. The combination of inflammation and ulceration can cause abdominal discomfort and frequent emptying of the colon. Ulcerative colitis is the result of an abnormal response by your body's immune system.
What is gastroesophageal reflux disease (GERD)? What are the complications of long-term GERD?
Gastroesophageal reflux disease (GERD) can be thought of as chronic symptoms of heartburn. The term refers to the frequent backing up (reflux) of stomach contents (food, acid, and/or bile) into the esophagus-- the tube that connects the throat to the stomach. GERD also refers to the array of medical complications, some serious, that can arise from this reflux.
Long term complications of GERD are:
- Oesophagitis,
- Barrett's Oesophagus,
- Cancer of the Oesophagus.
Read Shivaji's journey: I triumphed over Oesophagus Cancer
Oesophagitis, or inflammation of the esophagus, is a complication of GERD. If GERD is left untreated, oesophagitis can cause bleeding, ulcers, and chronic scarring. This scarring can narrow the esophagus, eventually interfering with your ability to swallow.
One major complication which occurs in about 10% to 15% of people with chronic or longstanding GERD is Barrett's Oesophagus. Barrett's Oesophagus results when the normal cells of the esophagus are replaced with cells similar to those of the intestine. This increases the risk of esophageal cancer. Developing Barrett's Oesophagus does not mean you will get cancer, but your chances of getting cancer will be greatly increased. Your doctor will want to check you on a regular basis in order to detect any cancer in its early stages. People who have Barrett's Oesophagus may require periodic endoscopies with esophagus biopsies to check for pre-cancer cells (dysplasia).
What is Celiac Disease? What are its symptoms and causes?
Celiac disease is an autoimmune disorder that can occur in genetically predisposed people where the ingestion of gluten leads to damage in the small intestine. It is estimated to affect 1 in 100 people worldwide.
Celiac disease -- also known as celiac sprue or gluten-sensitive enteropathy -- is a digestive and autoimmune disorder that results in damage to the lining of the small intestine when foods with gluten are eaten. Gluten is a form of protein found in some grains. The damage to the intestine makes it hard for the body to absorb nutrients, especially fat, calcium, iron, and folate.
Causes of Celiac Disease
Normally, the body's immune system is designed to protect it from foreign invaders. When people with celiac disease eat foods containing gluten, their immune system forms antibodies to gluten which then attack the intestinal lining. This causes inflammation in the intestines and damages the villi, the hair-like structures on the lining of the small intestine. Nutrients from food are normally absorbed by the villi. If the villi are damaged, the person cannot absorb nutrients properly and ends up malnourished, no matter how much he or she eats.
Symptoms of celiac disease vary among sufferers and include:
- Digestive problems (abdominal bloating, pain, gas, diarrhea, pale stools, and weight loss)
- A severe skin rash called dermatitis herpetiformis
- Iron deficiency anemia (low blood count)
- Musculoskeletal problems (muscle cramps, joint and bone pain)
- Growth problems and failure to thrive (in children)
Click here to get a complete understanding of Celiac Disease.
What are some of the risk factors for developing pancreatic cancer?
No one understands the underlying causes of pancreatic cancer, but certain risk factors have been identified. These factors are present more often in people who get pancreatic cancer than in people who don't.
There are multiple pancreatic risk factors, although most are only weakly associated with the disease. Many people with pancreatic cancer don't have any one specific risk factor.
About one in 76 people will develop pancreatic cancer. This represents the average risk of the condition. People with any of the risk factors are at slightly higher risk than the general population:
- Genetics. Five percent to 10% of people with pancreatic cancer have an immediate family member who also had it. Several different genes have been associated with the increased risk, although no "pancreatic cancer gene" has yet been identified.
- Diabetes. People with diabetes are not necessarily more likely to get pancreatic cancer but the two have been linked.
- Smoking. Cigarette smoking is well known to increase the risk for pancreatic cancer. The more a person smokes, the higher the risk. Ten years after quitting smoking, the risk returns to about that of someone who never smoked.
- Obesity and inactivity. In a study of 88,000 nurses, those who were obese (body mass index higher than 30) were more likely to develop pancreatic cancer. Those who exercised frequently were about half as likely to get pancreatic cancer, compared to those who did not exercise at all.
- Diet. A diet high in fat and meat (especially smoked or processed meat) has been linked to pancreatic cancer in animal studies. Eating a healthy diet rich in fruits and vegetables decreased pancreatic cancer risk in other studies. Still other studies suggest there's no identifiable link between diet and pancreatic cancer.
- Lycopene and selenium. Studies have shown low levels of these nutrients in some people who developed pancreatic cancer. That's not proof that low levels of lycopene and selenium cause pancreatic cancer, though. Any diet that includes lean meat and red or yellow vegetables should provide adequate lycopene and selenium.
What are colorectal polyps?
A colorectal polyp is a polyp (fleshy growth) occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.
Colorectal polyps are often classified by their behaviour (i.e. benign vs. malignant) and/or etiology (e.g. as a consequence of inflammatory bowel disease). They may be benign (e.g. hyperplastic polyp), pre-malignant (e.g. tubular adenoma) or malignant (e.g. colorectal adenocarcinoma).
Types
- Hyperplastic polyp
- Neoplastic polyp
- Adenomas
- Hamartomatous polyp
What dietary and other lifestyle changes should one follow to reduce risk of colorectal polyps or colorectal cancer?
Following are the risk factors enlisted of colorectal polyps or colorectal cancer:
- A personal or family history of colorectal cancer or polyps
- A diet high in red meats and processed meats
- Inflammatory bowel disease (Crohn's disease or ulcerative colitis)
- Inherited conditions such as familial adenomatous polyposis and hereditary non-polyposis colon cancer
- Obesity
- Smoking
- Physical inactivity
- Heavy alcohol use
- Type 2 diabetes.
So as to reduce the risk of colorectal polyp or colorectal cancer following factors in terms of dietary and lifestyle changes that need to be taken care of are:
- A good balanced diet and healthy lifestyle.
- Regular physical activity / exercises.
- Avoid eating red meat.
- Avoid smoking and alcohol consumption.
- To keep a good check on diabetes.
- Taking a proper treatment for the ulcerative colitis/crohn’s disease.
- Weight reduction in case patient is overweight.
- In case of family history of colorectal cancer or adenomatous polyposis, need to take preliminary care of all above mentioned factors and a mandatory annual routine gastro checkup for screening of early cancer.
What is chronic pancreatitis? What are its main causes?
Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis.
Causes of Pancreatitis are:
- Alcohol
- Autoimmune disorders
- Intraductal obstruction
- Idiopathic pancreatitis
- Tumours
- Ischemia
- Calcific stone
Are gastrointestinal disorders a common occurrence with individuals with Autism?
Gastrointestinal disorders in persons with Autism are:
- Gastritis
- GERD
- Colitis
- Irritable Bowel Syndrome
- Constipation
- Motility-based disorders
- Food allergy and sensitivity
- Overgrowth syndromes
Food allergy in this population is common - food allergy can affect any site in the GI tract.
Could you suggest 5 healthy tips to prevent gastrointestinal problems?
- Have a healthy balanced and lean diet along with a good amount of raw foods and probiotics for a healthy gut.
- Eat on schedule daily and have an early dinner - a gap of at least a minimum of 2/3 hours before going to bed.
- A regular exercise routine along with some yoga and meditation for inner healing and a healthy life.
- Skip all the bad habits: Smoking and avoid excessive caffeine and alcohol.
- Everything in moderation – Mind over body – Do not ignore your GUT feeling
Dr Vipulroy Rathod is the pioneer of Interventional Pancreato-Billiary EUS (Endoscopic Ultrasound). Having performed more than 18,000 EUS Procedures and over 35,000 diagnostic and therapeutic endoscopic procedures has earned him the distinction of the largest individual experience in advanced endoscopy in the Indian subcontinent. He is the first Indian Endoscopist to be awarded a Fellowship of the American Society of Gastrointestinal Endoscopy (FASGE). He has more than 25 articles and abstracts published in national and international journals of endoscopy. Dr Rathod is the Promoter and Director of Endoscopy Asia, a State of the Art Tertiary Care Facility in Gastroenterology, Hepatology & Endoscopy and has also set up the World Gastroenterology Institute (WGI), the first gastroenterology hospital of western India.