Porrselvi A.P. a cognitive and psychosocial interventions specialist shares the six common migraine triggers for men and women. And what you should do to pro-actively manage your migraine.
Migraine is a severe, recurring and throbbing pain, usually on one side of the head. It is a chronic neurological disorder in which a throbbing, pulsating type of headache is only a symptom. Migraine is actually caused by the uneven vasodilation of the cranial blood vessels (expansion of the blood vessels in the brain), while isolated headaches are usually not caused by the same processes as migraines. During a migraine, there is an inflammation of the surrounding brain tissue which increases the pain.
अब हिंदी में पढ़े: 6 मुख्य माइग्रेन ट्रिगर्स और माइग्रेन का सक्रीय रूप से प्रबंधन
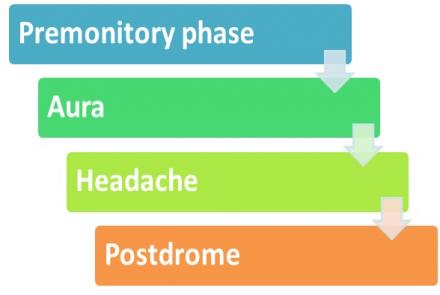
Unlike an isolated headache, Migraine has many symptoms like nausea, vomiting, auras (light spots), sensitivity to light and sound or smell, weakness, numbness, dizziness, difficulty in speech etc. Migraine is severely disabling as one migraine attack can sometimes last for eight hours to even several days. The headache can be so severe sometimes that the person will have to lie still in a darkened room until the episode subsides. The duration that someone is affected by an attack is actually longer than the migraine itself, as there is a premonitory or prodrome phase, a headache phase and then a postdrome phase in any migraine attack that can last one to two days.
There is also a type of migraine called the silent migraine in which there is no headache but only other migraine symptoms including an aura.
Types of Migraine
Migraine is divided into two major subtypes: Migraine without aura (MWOA) and Migraine with aura (MWA). Migraine without aura is the most common form of migraine. An aura occurs before the headache during the prodrome phase. Aura does not occur in all people with migraines. Visual aura are the changes in vision that a person may experience when they have a migraine attack. Patients may report seeing flashes of light, bright spots, lines or patterns of light just before the headache. The aura symptoms don’t necessarily have to occur with each and every migraine attack. About one-tenth of migraine sufferers complain of sensory aura, that is, an aura which involves senses other than vision. The symptoms of sensory aura usually include numbness, tingling and other “odd” sensations in the limbs, face or throughout the body.
Triggers of Migraine
A trigger is anything in the environment or any bodily change that may cause a migraine attack. The triggers required to cause a migraine attack is different for each person. Migraine can be induced by various controllable and uncontrollable triggers. Uncontrollable triggers include weather patterns and menstrual cycles, and controllable triggers include bright lights, strong perfume, noise, inconsistent sleep patterns, dehydration, hunger, fasting, jaw grinding, certain foods, exercise, alcohol intake etc.
We talk of some of the common migraine triggers:
1. Stress
There has been a lot of research on the role of stress in migraine and it has been proven that stress does trigger migraine in many people. Many people report that their first migraine attack was following a major stressful event in their lives, such as a death or a divorce. Stress can make a migraine attack worse or make migraine attacks last longer or more frequent. Sometimes migraine attacks can occur immediately after a very stressful situation is dealt with, that is right after a sudden release of tension due to the changes in the level of cortisol in the body.
2. Contraceptive Pill
Migraines are more common in women than in men especially during the reproductive years. This is attributed to the role of the female sex hormones like oestrogen and progesterone which implicates the menstrual cycle as a significant migraine trigger of migraine in women.
Some contraceptive pills contain oestrogen type components and this will have an effect on migraine as it can be triggered by a drop in oestrogen levels. Such a drop in oestrogen level can occur naturally through the menstrual cycle or can occur during the week when you do not take the pill between two OCP cycles. So it is important to consult with your doctor which type of oral contraceptive pill suits you based on your risk factors or to choose non-hormonal methods of contraception.
3. Pregnancy
Migraine often improves during pregnancy due to the lesser fluctuation of hormonal levels during pregnancy as compared to the monthly fluctuations in a non-pregnant woman especially in women who used to get migraines without aura (70%). This improvement may also be due to the increased levels of endorphins in pregnancy.
But for some women, migraine attacks can occur unchanged, or rarely may even get worse. Immediately following pregnancy, migraine can go back to how it was before pregnancy but breastfeeding women may be protected against migraine due to stable oestrogen levels.
4. Exercise
Regular moderate physical exercise has a therapeutic effect on migraine. On the other hand, strenuous exercise is also known to be a trigger for migraine. Therefore it is necessary to plan your exercise regimen and type of exercise you want to do based on your body requirements. It is necessary to have healthy diet with adequate food before exercise (hunger and hypoglycemia can trigger migraine), make sure you are not dehydrated before, during and after exercise, warm up and stretch first, don’t do strenuous exercise and do not exercise in high altitudes or in hot and humid conditions.
5. Chocolates and Caffeine
Migraine patients often say that a strong cup of coffee helps them during an attack. Caffeine's effect on the brain varies depending upon how often you take it. With occasional intake, it may provide modest acute headache relief. However, with frequent caffeine exposure, the brain may develop a tolerance for it. This means that it becomes less effective with repeated use. Many research studies have reported that contrary to the commonly held belief of patients and physicians, chocolate does not trigger headaches in typical migraine, tension-type, or combined headache sufferers. On the other hand, chocolate can promote the release of endorphins which may play a protective role in migraine.
6. Obesity
The association of migraine with obesity has been studied and it has been reported that the risk of migraine increases with increasing obesity and changes in body weight may affect headache frequency. Abdominal obesity may be associated with a greater risk of severe headaches and migraine in reproductive-aged women than men. Lack of physical activity has been demonstrated to be associated with a 21% increased risk of headache attacks in adults with migraine and a 50% increased risk of migraine in adolescents. Risk of migraine showed almost 40% increase in women with either general or belly obesity and almost 40% increase in men with general obesity and 30% increase in men with belly obesity as compared to those who are not obese. The association of obesity to migraine is hypothesized to be due to products produced in the hypothalamus (Serotonin and orexin that regulate food intake and also play a role in migraine) and the fat cells (Adiponectin and leptin play a role in inflammation in migraine).
How to Manage Migraines
- The first and most important step in managing migraines, after a diagnosis from a doctor, is to stick to your prescribed drug regimen and follow it diligently
- The next step is trigger identification. A qualified therapist can help you in understanding and identifying the environmental and bodily changes that trigger your migraine attacks and help you maintain a migraine journal if required.
- Once the triggers are identified, the therapist can help you facilitate a healthier body and environment for yourself so that the frequency and severity of migraine attacks will reduce. This can include cognitive and psychosocial interventions that help remove or diminish the effect of the identified trigger on you.
- Stress is known to be a significant trigger for headaches and migraines for many people. Better stress management and anger management skills can help in the management of migraine. Relaxation techniques like deep breathing exercises, emotive imagery, progressive muscle relaxation, mindfulness meditation can also help.
- For patients who are unable to quit alcohol or smoking when those habits are identified triggers for their migraine attacks, a qualified therapist can help them with de-addiction.
- Migraine patients are more likely to have depression and anxiety. Safe and effective drug and behavioural treatments are available for depression and anxiety. A qualified professional will be able to diagnose and help you.
- Better sleep hygiene and sleep behaviours can help in reducing migraine frequency and severity. Some of the healthy sleep behaviours are as follows:
- A consistent bedtime that allows 8 hours time in bed
- Not watching TV, reading or music in bed
- Not using mobile phones or other electronic gadgets in bed
- Avoiding or limiting caffeine, nicotine and alcohol at bedtime
- Use visualisation techniques to shorten time to sleep onset
- Moving your last meal time to at least 4 hours before bedtime
- Limiting fluids within 2 hours of bedtime and avoiding short naps.
Many patients with migraine say they feel they are forgetful or cannot concentrate on tasks at hand when they have an attack. Though research on cognition in migraine is inconclusive, it is best to seek professional help if you feel you are not able to cognitively function as good as you used to before.
Migraines are not Headaches!
Migraine can cause marital and family discord as the rest of the family may not understand the difficulties that the patient may go through. These misunderstandings may lead to arguments which may further add to emotional stress and trigger migraine attacks. Patient and caregiver education sessions with a qualified professional can help in dealing with this issue.
When such proactive therapy with a qualified therapist is combined with prophylactic migraine medication and optimized acute medical therapy in the event of a migraine attack, it can significantly improve the quality of life for people with migraine than with medication alone.