And other such questions on Migraine addressed by Dr Amit Haldar, Head of Neurology at Medica Superspeciality Hospital, Kolkata. He also tells us about the role of triggers and the best way of avoiding migraines.
Is migraine the same thing as a common headache? If not, how does it differ?
Migraine is an episodic hemicranial (one-sided) throbbing headache. It has got definite diagnostic criteria that include intolerance to light and sound. There may be associated issues like nausea and vomitting as well. There is no medical condition called common headache. It may sometimes be a common term to actually mean migraine. There could be other causes like tension, which could also lead to headaches. A headache is usually a symptom, and not necessarily a disorder.
Click Here To Read Or Listen To This In Hindi
How debilitating can a migraine be? What is the worst case you have come across?
The severity of migraine is widely variable. If on a visual analogue scale a patient is asked to mark the severity of his attack, most people will mark it as moderate (5 on a scale of 10).
However, there are people who have very severe and incapacitating attacks (9 or 10 on the same scale). These people have to sometimes visit the emergency units. I have had to admit a few of these patients and control their pain with intravenous medicines.
What are the most common triggers of migraine?
Migraine is a neurological disorder which can sometimes be aggravated by lifestyle choices. The triggers in our country are not the same as those in Western countries. There are some universal migraine triggers like fasting, sleep deprivation, stress, alcohol, smoking. Strain on the eyes is increasingly becoming a cause as well because of the continuous use of computers and video screens in the present times.
Cheese, wine, chocolate, excess caffeine, smoked fish or cold salads are known to cause migraine.
In a tropical country like India, hot humid weather, loud noise and bright lights are usually the common triggers. ”Hairwash headache” is something common in Indian women, due to the prevalence of long hair and not drying it well. Certain food additives like glutamate (MSG present in Chinese food) or aspartame are also often the triggers.
Do the triggers generally differ between men and women, or are they highly individualistic?
For women, hormonal changes can trigger an attack. Oral contraceptives should also be avoided by women who suffer from migraines. This is because oral contraceptives commonly contain estrogen and estrogen is a hormone that can aggravate migraine.
Is migraine hereditary?
Migraine is a complex genetic disorder where the genes interact with environmental factors to manifest. Twin studies have shown that the risk of inheritance varies from 34-51%. A child with one parent who suffers from migraines has about a 50 per cent risk of developing migraines. If both parents have migraines, the child’s risk goes up to 75 per cent. This risk is more in migraines with aura and familial hemiplegic migraines.
In 2010, a gene called TRESK was found to be directly linked to a common type of migraine.
Do children suffer from migraines? What are the signs that parents should look out for?
Children can suffer from migraines just like adults do. However, the manifestations are not the same. They can probably complain about headaches. However, sometimes vertigo may also be the main symptom (Benign paroxysmal vertigo of childhood). For some children, it may manifest as episodic abdominal pain or even vomitting (Abdominal migraine or Cyclic vomitting of childhood). This may result in acute confusion or neck deviation.
This poses a diagnostic challenge to the parents as well as the paediatricians. Any unexplained episodic repetitive event should warn the parents to consult a doctor. They also have to be aware that vertigo, vomitting and abdominal pain can also be features of childhood migraine.
What exactly is a combination of triggers? What is the best approach to identify one’s own triggers?
We have already discussed the triggers for migraine. However, for most it is rarely just one trigger. Usually, it’s a combination of factors. Individually, perhaps, they can be tolerated, but when several triggers occur together or accumulate, a threshold is crossed and an attack is triggered.
I advise my patients to maintain a migraine diary. There they write down the dates as to when they have their headaches and the possible triggers associated with the attacks. They then compare it with a standard trigger checklist. After a few months, they can themselves identify their own triggers and modify lifestyle accordingly.
What are the complications of migraine? What are the red flags which indicate the need for further investigations?
Migraine attacks usually don’t have any long term medical complications. While this is reassuring, one should be aware of the entity called medication overuse headaches. Excessive use of over the counter medicines can make migraines refractory and chronic. Analgesics can damage the kidneys and cause peptic ulcers. Moreover, improperly treated migraines run the risk of transforming into chronic daily headaches with devastating consequences.
Normally, migraines can be diagnosed clinically.And it does not require any investigation. But there are some red flags or warning signs that mandate investigation in a migraine patient.
These are-
- Thunderclap Headache: Very severe headache that reaches its maximum severity immediately (within a couple of minutes). Thunderclap headaches require emergency medical evaluation.
- Positional Headache: Headache that substantially changes in intensity in association with changes in position – e.g. standing from lying or viceversa.
- Headaches Initiated by Exertion: Headache starting while coughing, sneezing, and/or straining.
- New Headaches: Especially if older than 50 years of age, or if there are medical conditions that make worrisome headaches more likely (e.g. cancer, blood clotting disorder).
- Substantial Change in Headache Pattern: Significant increase in headache frequency or significant change in headache characteristics
- Constant Headache Always in the Same Location of the Head
- Worrisome Neurologic Symptoms: Headache that never goes away. Usually the aura of migraine lasts less than one hour.
- Systemic symptoms,including fever, chills, weight loss, night sweats.
Can migraines be prevented? What are the best ways to pro-actively prevent migraines?
The best way to prevent migraine is to avoid the triggers.
However, if the attacks occur inspite of avoiding triggers, medicines are needed. These are prophylactic medicines. They may include Flunarazine, Amitryptiline, Topiramate, Propanolol or Divalproex Sodium. However, these medicines should be taken under medical supervision for a minimum period of 3-6 months.
Sometimes, only medicines are not sufficient. Modification of the risk factors will add to the effect of medicines.
Related Reading: Pro-active Management of Migraine
What steps can a person take during the prodromal phase to manage migraine?
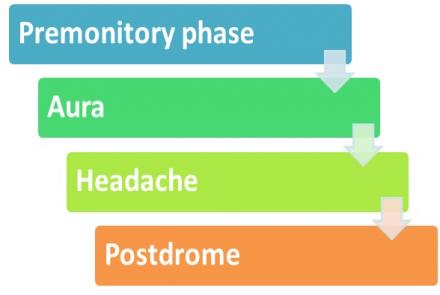
Prodrome is the phase immediately before a migraine attack.. A person may have mood swings or irritability during this period. Rest is the most important measure that a person can take during the prodrome. If the trigger is known, try to avoid it.There are some rescue medicines that can also abort an attack. They should be given only during the aura and not during the prodrome.
What non-pharmacological treatments help in the case of migraines?
As migraine can increase with bad lifestyle habits,it usually helps to avoid triggers.. Most important is reduction of stress. Adequate sleep , rest and diet can also help. Yoga and relaxation techniques can help in stress management.
Index
- ‘Hair wash’ or ‘head bath’ triggering migraine – observations in 94 Indian patients K Ravishankar
- http://thejcn.com/Synapse/Data/PDFData/0145JCN/jcn-1-
- https://americanmigrainefoundation.org/understanding-migraine/headache-red-flags-when-to-see-your-doctor/