
Malnutrition is seen in patients who have chronic or critical illness due to hospitalisations and post-surgical procedures. Enteral and parenteral are two of types of clinical nutrition prescribed by physicians. Dr. Shital Raval Patel unpacks this topic so we can understand the role of clinical nutrition, the types and how to handle these at home keeping patient safety front and centre
What is clinical nutrition?
The European Society for Clinical Nutrition and Metabolism defines clinical nutrition as ‘a discipline that deals with the prevention, diagnosis and management of nutritional and metabolic changes related to acute and chronic disease and conditions caused by a lack or excess of energy and nutrients’. It is essentially a special area of nutritional science that focuses on management of diseases by providing nutritional therapies, correcting micronutrient deficiencies and protein insufficiency and preventing chronic diseases.
Why is clinical nutrition important?
The body requires nutrients for all of its processes, development, growth and for energy. Lack of essential nutrients basically causes malnutrition. Malnutrition is seen in patients who have chronic or critical illness due to hospitalisations and post-surgical procedures. Metabolic processes slow down and organ functioning will eventually start getting affected. The immune system grows weak impairing the body’s responses to foreign infections.
Hence administration of early nutrition is key to speedier recovery and better health outcomes with minimal to no complications of malnutrition. Benefits to the body include:
- Proper gastrointestinal functioning
- Normal bowel motility and movements
- Healthy bladder and urine output.
- Decreasing chances of infection by keeping the normal flora (normal healthy bacteria) in check
- Improving wound healing
- Faster recovery of body systems
- Fewer days in the hospital
Besides nutrition, fluid and electrolyte intake are equally important for the body. The balance of all these is necessary for proper functioning. Any imbalance in the ratio of nutrients, oxygen and water can result in dehydration, constipation, urinary tract infections etc.
Types of clinical nutrition?
The delivery of medical specific nutrition is done via two channels namely enteral (via mouth or tube) or parenteral (via IV).
- Enteral nutrition refers to nutrition administered via the gastrointestinal tract. It may be done orally or via tube feeding. If for any reason, the patient is unable to eat orally, then tube feeding or parental options are explored.
- Parenteral nutrition (PN) refers to nutrition administered into the intravenous system (into a vein) thus bypassing the gastrointestinal tract. The nutrition consists of a specially prepared liquid mixture consisting of all major food components i.e. protein, carbohydrates, fats, vitamins, minerals, and other nutrients essential to the body. This method of food delivery is opted for when oral and tube feeding are not possible or contraindicated for the patient.
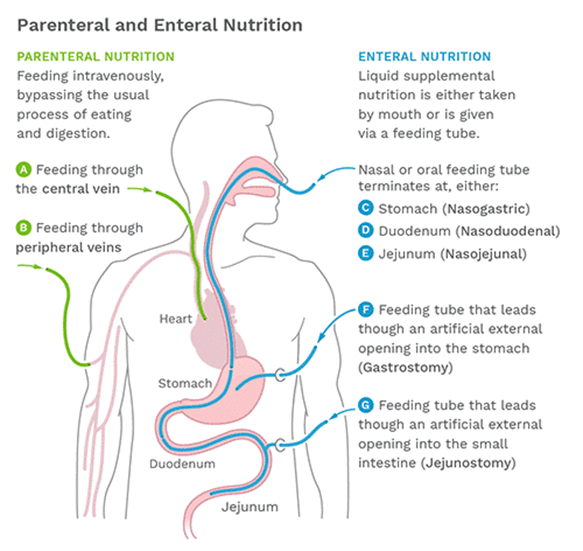
Figure courtesy of Crohn’s & Colitis Foundation, www.crohnscolitisfoundation.org
Enteral Nutrition via Tube feeding
Types of feeding tubes:
Your doctor will decide which type of tube is best for you. The decision on which type of tube should be inserted is from the following options:
- Nasogastric (NG) feeding tube
- Naso jejunal (NJ) feeding tube
- Gastrostomy tubes such as percutaneous endoscopic gastrostomy (PEG) or radiologically inserted gastrotomy (RIG).
- Jejunostomy tubes such as surgical jejunostomy (JEJ) or percutaneous endoscopic gastrostomy (PEG-J).
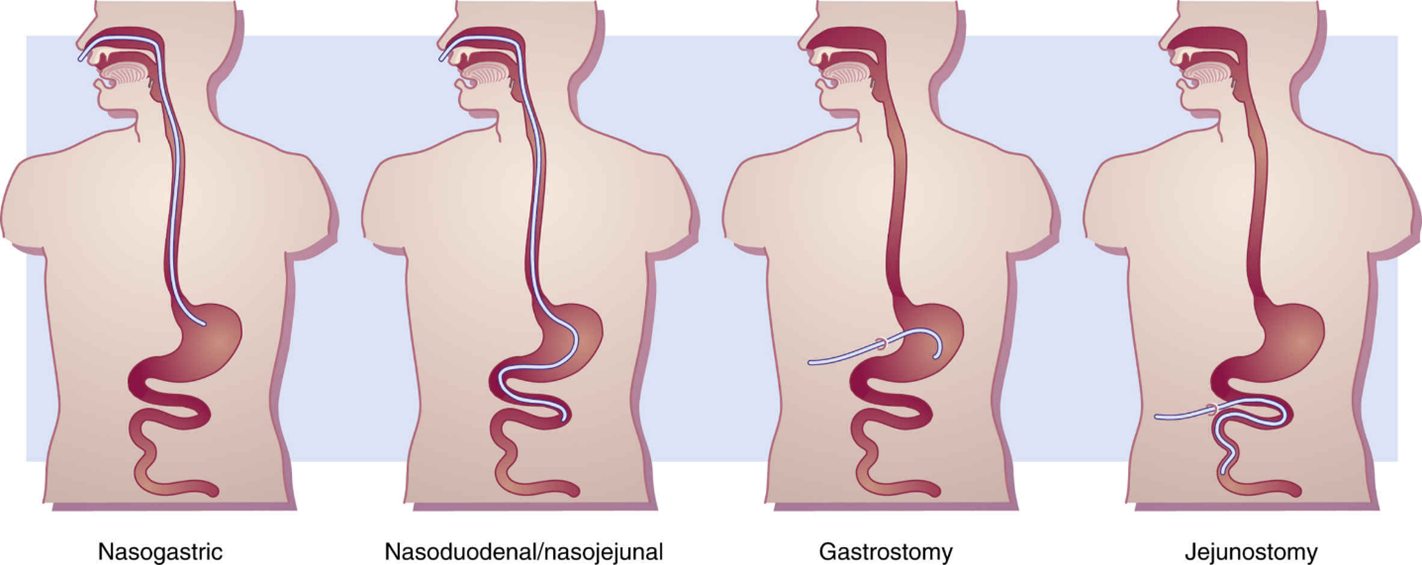
Figure Courtesy of https://basicmedicalkey.com/nutritional-support-2/
| Type of Tube | Route of Tube | Indication |
| Nasogastric (NG) | Inserted from the nose to go down to the stomach | Used for short-term such as 6 to 8 weeks |
| Naso duodenal/jejunal (NJ) | Inserted from the nose to go down till the small intestine | Used when feeding into the stomach is not tolerated |
| Gastrostomy (PEG or RIG) | Inserted directly into the stomach from outside. | For longer term use such as more than 6 weeks. |
| Jejunostomy (JEJ or PEG-J) | Inserted directly into the small intestine from the outside | For longer term use such as more than 6 weeks. |
Complications of Enteral (Tube) feeding
Patients and their care providers should be made aware of some of the complications that may occur due to tube feedings. These include
- Dehydration is a common problem faced by patients on enteral nutrition. High protein content and inadequate fluid intake can easily cause dehydration.
- Aspiration pneumonitis is a serious and life-threatening complication. It can occur due to reflux of feed into the airways and into the lungs. One must watch for signs of coughing, wheezing, respiratory distress in patients. This can be prevented by keeping head elevated during feeds and checking the gastric residual volume.
- Diarrhea is seen in many patients. Causes can be rapid feeds, low-fiber feeds and tube movement and contamination of the feed or tube. Make sure food preparation and tube hygiene is ensured. Inform your doctor if diet is lacking sufficient fiber.
- Refeeding syndrome is a consequence of multiple issues that occur when malnourished or starved patients receive rapid refeeding. The imbalance in the electrolytes and fluid causes changes in glucose, protein and fat metabolism along with disruption in hormonal and metabolic processes.
Therefore, patients who are receiving tube feeding must be monitored closely to make sure there is no imbalance in the nutritional requirements. This is usually done by testing the blood and looking at any variations in certain key parameters such as the electrolytes (potassium, sodium etc.), blood glucose levels, blood urea nitrogen (BUN), creatinine, serum proteins etc.
Measurements of blood pressure and weight need to be carried out regularly. Frequency of monitoring will be decided by your doctor.
Patient Safety in Enteral Nutrition
Administration and care of the feeding tube plays a big part in patient safety. The role of the nurse or care provider become important is ensuring this. Certain key points regarding safety of the patient are:
- Position of the patient: The patient’s head must be elevated by 30-45 degrees during feed time and for 30-40 minutes after feeding has completed. If patient cannot elevate his/her head, then the bed/mattress should be elevated. Risk of Aspiration is decreased by elevation of the head during and after feeds.
- Position of the tube : Always check the position of the tube before initiating feed. Make sure the tube has not moved, and is in place. Change the masking tape that hold the tube to the skin daily so it does not come off. It is likely to become wet if it gets wet during cleaning or showering.
- Tube hygiene: make sure tube looks clear and transparent. If there is any feed stuck in the tube, flush it with saline or water.
- Gastric Residual volume (GRV): Patients with acute illnesses may be unable to empty their stomach easily. During feeds, if the stomach fails to empty its contents, it can cause feed to rush back into the esophagus creating reflux. If content flow back higher and pass into the air pipe, it can even cause aspiration pneumonia. One way to prevent this is to monitor the residual volume and adjust the speed of the feeds accordingly. GRV should be checked every 4 hours in the first 48 hours of tube insertion by a nurse.
- GI functioning: Assessment of the whether the nutrition is being digested and absorbed can be done by listening for audible bowel sounds by placing ear to the abdomen or by auscultation. Check if the patient is having normal and regular bowel movements and urinary output. Patients should be assessed for any signs of dehydration.
Parenteral Nutrition types
Can be Partial or Total. Partial nutrition is given when a patient is receiving some feeding (could be enteral or oral) but still has some malnutrition. Total is complete delivery of nutrition to patients whose digestive systems are unable to accept oral foods and digest them.
The IV tube is inserted in either the superior vena cava or a smaller vein in the neck or arms. The location of IV classifies the parenteral nutrition into 2 types:
- Central parenteral Nutrition or CPN: Here the IV is inserted into the superior vena cava, a huge vein that goes straight to the heart. Since it is a large vein, Total nutrition is delivered through this system as a bigger catheter can be put in.
- Peripheral parenteral nutrition or PPN: When smaller or temporary nutrition needs to be delivered, this system is used. IV is inserted into smaller veins of the neck or arms, making it ideal for Partial parenteral nutrition.
Complications of Parenteral (IV) feeding
- Risks associated with insertion of the catheter in Central parenteral nutrition. These include pneumothorax, air embolism, bleeding, thrombosis/clots, and damage to the vein.
- Infection of the catheter; this can be local at the site of the IV insertion, or in the bloodstream which is potentially more dangerous.
- Metabolic problems such as:
- Changes in blood glucose levels leading to hypo or hyperglycemia.
- Liver disease (fatty liver, NAFLD) is seen in patients with long-term parenteral nutrition.
- Gall bladder problems due to the accumulation of bile.
- Reduced bone density from deficiencies in calcium, magnesium, and Vitamin D.
- Abnormalities in electrolytes.
- Refeeding syndrome usually seen in severely malnourished patients within the first few days of starting refeeding. Symptoms include nausea, vomiting, and diarrhea due to several metabolic changes in the body.
Patient Safety in Parenteral Nutrition
Since parenteral nutrition is considered more complex, close monitoring and nutrition guidelines must be followed. Usually, parenteral nutrition is managed by a team consisting of your treating doctor, nurse and dietician at the hospital. The team will also help the patient transition from parenteral to oral nutrition at the right time. If parenteral nutrition is managed at a home setting, a nurse will be the right person to manage the patient or train the primary care provider on how to do so.
References:
- Org, E. (2024, April 6). The European Society for Clinical Nutrition and metabolism. ESPEN. https://www.espen.org/
- Themes, U. (n.d.). Nutritional Support. Basicmedical Key. https://basicmedicalkey.com/nutritional-support-2/
- Yasuda, Hideto et al. “Monitoring of gastric residual volume during enteral nutrition.” The Cochrane database of systematic reviews vol. 9,9 CD013335. 27 Sep. 2021, doi:10.1002/14651858.CD013335.pub2
- Mehanna, Hisham M et al. “Refeeding syndrome: what it is, and how to prevent and treat it.” BMJ (Clinical research ed.) vol. 336,7659 (2008): 1495-8. doi:10.1136/bmj.a301
- Hartl WH, Jauch KW, Parhofer K, Rittler P; Working group for developing the guidelines for parenteral nutrition of The German Association for Nutritional Medicine. Complications and monitoring - Guidelines on Parenteral Nutrition, Chapter 11. Ger Med Sci. 2009 Nov 18;7:Doc17. doi: 10.3205/000076. PMID: 20049074; PMCID: PMC2795374.
- Hamdan M, Puckett Y. Total Parenteral Nutrition. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559036/






