Glaucoma is a leading cause of blindness in India. If managed well, you can prevent loss of vision and maintain a good quality of life.
PatientsEngage has partnered with IHOPE to bring to you insights on how to manage glaucoma effectively.
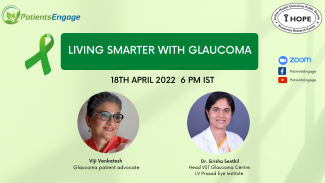
Our panelists for this discussion on 18th April were
Viji Venkatesh, Glaucoma patient advocate
Dr. Sirisha Senthil, Head VST Glaucoma Centre, LV Prasad Eye Institute
Dr. Sirisha Senthil, Head VST Glaucoma Centre, LV Prasad Eye Institute
Many people don’t understand this disease or know about it. Even members of the family don’t seem to understand or talk about it. They treat it like an accident. They think they will not get it or get into it.
Viji, a patient advocate says she works with cancer patients daily and has seen how beneficial it is to share experiences and learn from each other. “A medical condition isolates you and with isolation comes fear.” She feels that talking about the issues reduces the negative impact of the condition.
What is Glaucoma?
Glaucoma is a condition where there is damage to the optic nerve (the nerve that connects the eye to the brain), which is the most important part of the eye as it sends nerve impulses to the brain. There are no symptoms!
People slowly start losing vision due to elevated intraocular pressure and that leads to permanent vision loss or blindness. The condition is dangerous in 2 ways. One is people rarely experience any symptoms and when they do have symptoms, then it means it is already too late. The condition causes irreversible blindness, meaning vision loss is forever and nothing can bring it back. So, the only prevention is to bring about awareness and early diagnosis. The disease can be easily treated if detected early and vision can be preserved. However, late diagnosis is a big problem in our country. In the west, undiagnosed glaucoma is seen in 50% of the population, whereas in India it is seen in 90% as per the survey done by the LV Prasad Eye Institute and the Chennai Glaucoma study.
How and when should one get tested for Glaucoma?
Like most lifestyle diseases such as Diabetes or Hypertension, we must understand that incidence of glaucoma also increases beyond the age of 40. General advice is that when presbyopia sets in post 40 and one requires reading glasses, it is the best time to see an Ophthalmologist and get evaluated for glaucoma as well. This can also be done once every two years along with your eye glass prescription appointment. The test should be comprehensive with evaluation of the intraocular pressure and evaluation of the optic nerve. This is the simplest way to get checked for glaucoma.
Can an Optician do this evaluation or does one have to visit an Ophthalmologist?
Most optician shops will have an Optometrist present who can conduct this test. The major problem is that people do not have time for such screening. If they are able to read well with their glasses, they buy it and leave. A complete eye evaluation requires 1-2 hours where there is check-up of the front of the eye before dilatation and the back of the eye after dilatation. Without dilatation, only 30% of the eye can be seen as the back of the eye cannot be viewed. So ,glaucoma can be easily missed in the check-ups without dilatation.
Who should test?
Everyone post the age of 40 years. People who have a family history should test earlier depending on the type of glaucoma in the family. There is no fixed age so as a general rule, check-up at the time of onset of presbyopia is a good opportunity. For instance, patient with a family member with angle-closed glaucoma should start screening by age of 35 as it tends to occur in younger population.
Viji recalls that her mother had glaucoma and she would organise and accompany her to the eye clinics but never encouraged herself or her siblings to get an eye check-up. This wasn’t about the lack of time but the lack of awareness and self-care. It continues to be a big regret even today. She didn’t realise she needed any eye check-up until a lot of vision had gone. What alerted her was the realization that she was behaving such like her own mother with tripping, walking into glass doors etc. By the time, the eye check-up happened she was 58 years old. Though fairly young, her Ophthalmologist was upset about the delay in diagnosis. This motivated her to come forth and speak out and create awareness. She says, the only eye check-up most people get is the eye chart at the Optician’s and that is not enough!
What are the risk factors?
- Family history
- High myopia or short-sightedness is a condition linked to glaucoma especially open- angled glaucoma.
- History of trauma to the eye or intraocular surgery done at a young age.
- Indiscriminate use of Steroid drops and ointments on the face. Studies show that the commonest type of glaucoma in children is steroid-induced in India. LV Prasad Eye Institute published a paper in the British Journal of Ophthalmology that more than 50% of children at diagnosis were blind in one eye. This was primarily due to abuse of steroid drops for allergies, face ointments for dark spots, fairness creams which fail to mention they contain steroids etc. Use for even a short period of time such as a month or two can increase one’s risk of glaucoma. This is highly disturbing and has a huge impact on the child, the family and the society. In most countries, even small ones, steroids are not sold without a prescription. In India, it is available freely over-the-counter everywhere and for anyone. It is also cheap (Rs 8 per bottle) and provides quick relief.
Are people with autoimmune diseases who regularly use steroid at a higher risk?
Steroids as such are not bad when indicated, used appropriately by your treating physician and monitored regularly. Systemic steroids taken orally have minimal effects on the intraocular pressure but can cause cataracts. Drops and ointments used in and around the eye cause a higher risk of glaucoma. Even when applied on lips for eczema, they can enter the blood circulation and cause damage to the eye.
Viji recounts that both she and her mother were on Betnovate C for a skin condition.
Dr Sirisha reveals that she has seen many asthmatic patients on steroid inhalers have difficulty controlling their eye pressures. When the inhaler is substituted with another medicine, their pressures reduce. There is a term called Steroid Responsiveness, where some people are more susceptible to steroid side-effects than others. About 18-20% of people on steroids can be steroid responders.
What are the treatment options?
Treatment depends on the type of glaucoma one has. There are 2 basic types:
- Primary- is due to no other preceding cause. Can be hereditary as well when the drainage channels in the eye are not functioning as they shoul
- Secondary- is due to some other causes like trauma, surgery, steroid use etc.
- There are open-angle and angle-closure glaucoma. For angle-closure, laser is required to create fluid circulation pathway followed by medical treatment.
- For open-angle, majority are treated medically in the form of eye drops
- Once started on the treatment , it is to be continued lifelong unless they are operated for it and their intraocular pressures are under control.
How does glaucoma affect daily life?
Viji says she had to stop driving and riding her bicycle for safety reasons. She would trip and fall often. “If I looked down and walked, I would hit my head. If I looked up and walked, then it was all erratic on the floor level.” She also suffered from loss of peripheral vision and almost got hit by a car because she could not see from that side of the damaged eye. “I literally could not see where I was going!” Loss of depth perception made her clumsy and mindful of her movements. “I could not put anything down on a table properly”.
Viji had laser and was put on eye drops but wasn’t too compliant with them. It aggravated her condition and she had to undergo 2 more surgeries. She is now free of all eyedrops as her pressures have been brought under control after 8 years of treatment.
Dr Sirisha tells us that for 80% of the people, eye drops do work very well. For others, they may stop working or the disease continues to progress which then leaves the option of surgery for the patient. There are now multiple types of surgical interventions available. With new advances, an eye can be operated on several times to bring the pressures under control. Compliance with medications is very important and needed for this disease. Patients are advised not to stop or experiment with their eyedrops without the consent of their doctor.
Do medications cause darkening of the skin around the eye?
There are many medications available for glaucoma. One group of medicines is called Prostaglandin analogs, which are the commonest and most effective but can cause darkening of the skin near the eye. If this is a concern, speak to your doctor to replace the medication with another one. However, one should remember that all meds have some side-effect, so best to focus on the benefits. Some medications can also cause good side-effects like long eyelashes.
Tips for lifestyle changes
- Wear proper footwear with straps or buckles. Avoid heels.
- Walk slowly, take your time. Don’t hurry because our country is very disabled-unfriendly i.e. there are no railings, smooth floor tiles and stairs with varied depths etc.
- Be careful esp. on public transport. The bus steps tend to be very high, even rickshaws are not easy to get into.
- Do regular follow-ups with your doctor.
- Parties and social gatherings often have low dimmed lighting. Use your phone torch to help see better in such places.
- Change your environment since you cannot change your eye. Have more light when reading. Keep your surroundings well lit.
- Don’t change or move things around the house as one is often used to navigating them. Any change can cause falls. For the elderly, falls can be very dangerous.
Is there a particular time, when intraocular pressures are at their highest?
Pressures do fluctuate from time to time and can also depend on one’s hormones and metabolism. Generally, pressures peak at early morning.
Are there any diet recommendations?
Not really! Drinking water is the only factor that is helpful but avoid excessive water/liquid intake in one go or in a short span. This can overload your system and increase the intraocular pressure.
Are there any exercise recommendations?
Exercise is good for health. Some studies show that yoga and meditation can help decrease the intraocular pressure, possibly by action of the adrenal gland. However, one must not skip or stop their medications. Stress and worry can worsen your glaucoma due to increase in cortisol levels. Be careful with weight-lifting exercises especially after glaucoma surgery. During surgery the eye walls and muscles can become weak and any strain can be harmful. Essentially, any exertion that raises the abdominal and thoracic pressure like coughing, straining while passing stool, weight-lifting etc. should be avoided.
Viji points out that her doctor specifically told her to stop doing kapalbharti breathing as it is harmful for glaucoma.
What are some complications of glaucoma?
If pressures go uncontrolled, it can cause stroke and brain occlusion affecting the eye and lead to sudden loss of vision. It can cause cataracts earlier in life. Best way to prevent complications is to have the intraocular pressure under control.
What is the best time to take the eye drops?
There is no best time. Some medications are prescribed at night because the peak effect of the drop is between 4 to 5 hours after application, so this prevents that early morning peak in pressure. Some meds are given at night as they cause redness which you don’t want in the daytime. Some meds are given in the morning because they don’t work well at night when the body’s baseline blood pressure is low. Hence the medication is prescribed keeping in mind the mechanism of action and peak effect times of the drug.
Check out the video here: Living Smarter With Glaucoma
Changed
07/Apr/2025
Community
Condition






