
Jayesh Shah, who has been living with Type 2 diabetes is a very informed and aware diabetes patient. He has actively looked at ways to manage his diabetes better, be it in terms of trying diet changes or changing his exercise routine. When he read about Continuous Glucose Monitoring (CGM), he was keen to try it out. He shares his experience with CGM in detail.
Context:
I am a person living with Type 2 diabetes for over 30 years now. I was first diagnosed around the age of 29 during a routine medical checkup and am on medication from then on. For the first 18 odd years it was oral doses and then I was put on insulin shots. BTW, diabetes did not impede my lifestyle one bit. I have led and still do lead an active life, travelling the globe for work as well as pleasure. The one thing that changed of course, was my diet and later on, my exercise regime.
While my regular blood sugar test results – fasting, post prandial and HbA1c, dictated the changes in medication and dosage I was never sure what the sugar levels were in the period between those tests or were there any specific foods that caused spikes or was the interval between two meals causing hypo. Unfortunately, there was no way to figure that out and these remained questions in my mind – until now. Sometime in January this year, I chanced upon an article on the Internet that talked about CGM. I read it with a lot of interest and then started reading up more about CGM till I was convinced that I had nothing to lose in trying it out.
Trying CGM out:
The CGM device consists of a reader and sensor. The sensor, which lasts for 14 days, consists of a tiny needle that is to be inserted under the skin on the belly or arm. It measures interstitial glucose levels which is the glucose found in our cell fluids every few minutes. One has to just swipe the reader across the sensor at regular intervals to record the measurements. There are certain readers which even transmit data to mobile phones via an application.
The most important thing for me was to find a reliable reader whose sensors would be easily available in India. Once I had that figured out, I ordered a reader & sensor and was all set for the experiment.
Dr. Purvi Chawla, consultant diabetologist and director of clinical research at Lina Diabetes Care and Mumbai Diabetes Research Centre says:
Any type 2 diabetes patient may consider using CGM when they experience glycemic fluctuations and particularly hypoglycemia.
Even though recommendations say that CGM can be used by people with type 2 diabetes therapy on insulin and not achieving targets or experiencing hypoglycemia, it can be expanded to many situations in type 2 diabetes patients like fluctuations in sugars, to achieve better A1c control on oral drugs, to understand impact of lifestyle choices, to detect and prevent hypoglycemia, even in prediabetes and early diabetes to understand the impact of lifestyle.
Any patient using CGM must be trained and educated and supported by a healthcare professional.
There are at least 2 different types of Libre Pro continuous glucose monitoring (CGM) systems available, one being the professional version where it is a blinded CGM and the reader is with the health care provider and the CGM is read after 14 days or at least after 5 days and discussed with the patient, and the other one is the real-time one, which is what the patient appears to be describing. In India, the software to read it is not available but the reader can give the data and the same may be transferred to the phone or may be written down.
CGM from Dexcom is also available.
CGM testing may be undertaken once or twice a year as per availability, affordability and glycemic status.
Round 1:
I began using the device and tracking my sugar levels from the 27th of March 2021 till 10th of April, when the sensor expired. I recorded the measurements on an excel spreadsheet at hourly intervals (with some exceptions at night when I was asleep) and plotted a graph to see what was happening – I have reproduced the graph below which revealed some very interesting patterns. As you will see, I realised that my sugar level was going dangerously low between 2 & 3 AM and only going up once I had a small snack. Also, my post breakfast spike was too high while post lunch was almost within range. Another issue was the spikes post my evening snack and dinner which I figured was because of the very little time gap between the two.
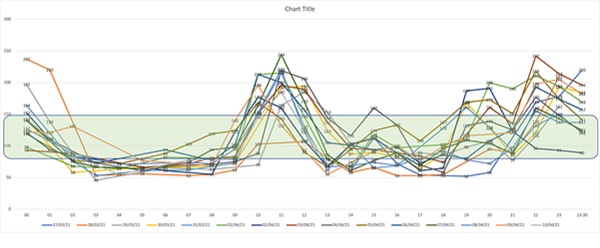
That said, my problem was that despite a very controlled, low glycemic dinner, my sugar level was spiking and more worryingly, was dropping very fast through the night to dangerously low levels. I spoke to my doctors and we tweaked the medication doses, time of medication and also made some diet changes based on the above data. We also decided that we will continue with monitoring the sugar using the glucometer for a while and then do another round of CGM after a couple of months.
Round 2:
Round 2 began on 10th of July 2021 and ended on 24th of July. I will break down my conclusions of this round in two periods – the first nine days and the next five days. The first period was based on my as-is medication and diet routine. See the graph below:
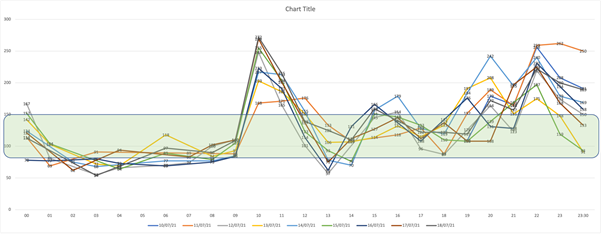
From the above, it is obvious that not much had changed despite the change to medication and diet routine. I realized that something more drastic needed to be done. So first, I completely cut out carbs from my breakfast – now it consists of a boiled egg and muesli with milk. Lunch remains the same, while the evening snack is had earlier to increase the gap between the snack and dinner. A significant change made was the timing of the insulin shot from pre-dinner to pre-breakfast. The graph below is for the five days post this change:
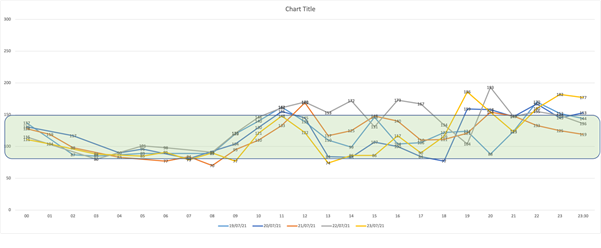
There is a noticeable difference in the sugar patterns with very few spikes and lows, which basically means that the sugar time-in-range (TIR) is good and most importantly, the lows in the night while asleep have disappeared. I am now continuing with the medication and diet routine which has given me the above results. Have planned Round 3 of CGM in the near future to see if this continues.
Post-script:
I would like to bring to the fore, the fact that there is a difference between blood sugar and interstitial sugar and one must use CGM only to discern the pattern and not rely on the absolute numbers.
For absolute numbers, please continue with lab tests, glucometer tests at home and the quarterly HbA1c.
Make sure you are in touch with your healthcare professional on the usage and findings of the CGM.
Another thing to be noted is that CGM systems are still relatively expensive. The reader is a one-time buy and can be reused any number of times. Only the sensor is a perishable item and has to be purchased for each round of testing.






