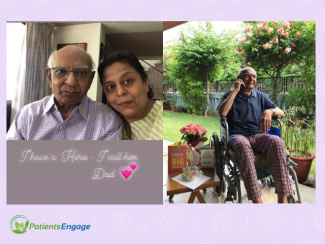
Prima shares the challenges of caring for her father who was diagnosed with stage 4 cancer of the ureter and kidney, the effect that COVID had on the treatment choices, the pain he went through, the palliative care choices and the emotional turmoil of it all.
I vividily remember that afternoon when he implored, “Take me to the doctor, I’m uncomfortable. I’m in pain and want to sleep”. My husband gave him his morphine pill and told him we would go see his doctor soon. He kept saying, he wanted to sleep, so I gave him his sleeping aid next. After he took the pills, he just lost his senses and his body went cold. He had finally just let go. He was 87 by then and had fought to live for 2 years.
My father, was diagnosed with ureter and kidney cancer just a year after my mom had passed away with colorectal cancer. By the time, he was diagnosed, it had already spread and was at stage 4. I flew down to India from my home in the US to be with him during his treatment. As a sole child, I had no choice but leave behind my family and take on a full-time role of a care provider. Luckily, my supportive husband and independent children made that possible for me.
Hip Fracture Complications
Due to his age, his each chemo was split into two, which meant 2 chemos per month and it would last 6 months. After his 3rd session, he developed sudden pain in his hip. A prompt CT scan showed that he had a hip fracture. His Oncologist suggested that he undergo surgery for either a complete hip replacement or one to just fix screws in place. My father refused both, he was not willing to go under the knife. He was clear, whatever will be will be. He soon realised that he could not walk and I had to organise a wheelchair for him even to move around at home. Getting onto a wheelchair was emotionally challenging for him as he came to terms with his loss of mobility. He mourned the loss of his independence along with the fact that he was now a burden. He eventually got used to it. I hired a male nurse to help me during the night and I was able to manage him during the day. Since, we had now moved him to the lower level of the bungalow, I could wheel him to his bed, the dining table and the bathroom. Once the fracture started to heal, he was able to use the walker too. Inspite of the fracture, his chemotherapy continued and we completed the treatment right around winter.

His hip had healed well and he was now walking slowly but confidently. The weather was good and I would often take him out for meals, we started meeting friends and family who we had put on hold all these months. We even had overseas and out-of-town guests who came to visit him including my kids and husband. Three months went by peacefully and joyfully.
Cancer Relapse
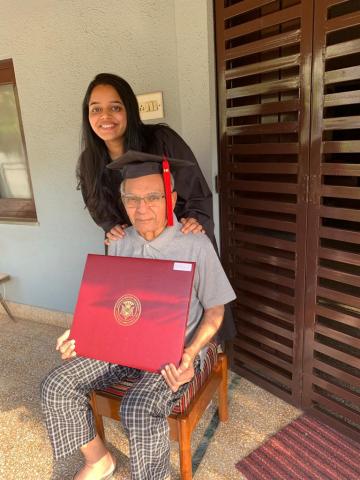
Our next follow-up revealed that his cancer had relapsed. Right abdominal pain had started because of new metastasis to his liver. It was most disappointing, because we were planning to go to the US for my daughter’s graduation. He was extremely upset that he would have to miss that. We did a whole video call so he could watch the ceremony from India but it would never be the same. He sorely missed his grandchildren and these milestones.
COVID complicates matters
Chemo was started immediately and just after his first session, Covid hit us. As the pandemic loomed over us, my husband flew down to be with us just in time before flights stopped. With my husband around, I was able to handle things as the helper had stopped coming because of the lockdown. With the intense fear of acquiring Covid by going to the hospital, we missed two Chemo sessions. Our Oncologist explained to us about the hazards of missing Chemo and so we resumed the sessions. Those Chemo days were not easy at all. After a long day at the hospital with masks and gloves, when we returned home, I would wash dad, give him his steam, sanitise everything again, put his clothes in Dettol and then finally go for a shower myself.
Side effects of Chemotherapy
The side-effects this time around also took a toll on us. He felt very weak, would barely get out of bed on most days and appetite has fallen. He has a history of Esophageal contraction or a narrowed esophagus which had made it harder for him to swallow food. Complicated with acid reflux, his food would go down and acid would push it back up. He has had this ailment since years but it seemed to have worsened with his cancer. Many a times he would take 5 minutes just to swallow one morsel of food. On bad days, he could eat just about 4 bites of his meal. He was completely on a soft food diet. A history of constipation and haemorrhoids did not help either. Chemotherapy had further made it worse. After some research online, I started him on a few daily diet regimes such as :
- Warm water with lemon in the mornings
- A shot of papaya leaf broth between meals
- Chas or buttermilk made with cumin, mint, tulsi and curry leaves with meals
- Soup made of beetroot, pumpkin or drumsticks
- Lots of water
This helped stabilise his digestive tract and made him comfortable while providing him with the right nutrients. During the Chemo, his hemoglobulin, potassium and sodium levels would often drop. He had a few saline and blood transfusions along the way. His heart was functioning well even though he had hypertension, hyperlipidemia, and minor valve leakage. He was put on a blood thinner and was well monitored.
Palliative Care
The gap of one month due to Covid had messed up his cycle. His body had become quite resistant to the chemo drugs. He started complaining of pain, severe weakness, uneasiness and discomfort. After his 4 session or so, he himself decided to stop the treatment. Palliative pain management commenced henceforth. We had a discussion with his doctor on how best to keep him comfortable. Tramadol and patches were prescribed along with a sleeping aid. On an SOS basis, morphine was prescribed but it caused a lot of drowsiness but no real sleep. So then he would ask for a sleeping aid, but because of the pain he just could not fall asleep. This deadly combination of pain, medications and insomnia resulted in delusions, incoherent talks, and nightmares. The last 2 months, he had lost control of his feet. Food intake had drastically reduced and some days, he would barely eat at all. Constipation was back but he would pass urine easily with his one functioning kidney. He would stay in bed all day, tossing and turning in states of consciousness. He would keep changing sides to find relief. If he fell asleep on one side for long, edema would develop on that side.
It was a lot of pain and he would keep complaining about it. We started using ice packs on his lower back for pain relief. His doctor now decided to give him morphine injections. The injections had just started when his body finally gave up.
My biggest challenge
Emotionally, it was very challenging. To see him deteriorate in front of me just broke me apart. Physically, I was determined to do whatever was needed to help my father. Single-handedly, I was ready to care for all his needs while being away for almost 2 years from my own family. But to watch him go through it all was shattering. He knew what the outcome was going to be but he wanted to enjoy his last few years of retirement. He also felt guilty about me being there away from my kids. He would often reminisce about my mother and the kind of pain she had gone through from cancer.






