A bedridden patient becomes vulnerable to various health complications like painful bed sores, circulation and respiratory problems, depression and contractures, due to lack of activity for long periods. Usha Ravi suggests steps to ensure proper nursing and caring for your loved one confined to the bed.
There are a host of challenges which arise if one is confined to bed because of sickness, disability or frail age. The burden is felt not only by the individual but also by the carers. It is important and beneficial for the carers to know what such individuals are going through and how they would like to be assisted.
This article addresses some of the common challenges and health risks of bedridden patients, and provides tips for the carers to prevent and manage those risks.
Some of the common complications:
- Pressures sores or decubitus ulcers
- Pneumonia
- Constipation
- Contractures (shortening and hardening of muscles)
- Deformity and Stiffness
- Recurrent Urinary Tract Infection (UTI)
- Depression
1. Pressure sores or decubitus ulcers
One of the most unfortunate and preventable complications that can occur are bedsores. Bedsores can develop in a person who is bedridden or immobile. Pressure laid on the skin and tissues that covers the bony areas of the body are at biggest risk for breaking down. This occurs from prolonged lying down or sitting in one position, compounded by poor nutrition, dry and wet skin, and shearing force on the skin as they are moved for change of dressing or clothes. The area under attack suffers from poor blood circulation, and shearing force rips the skin covering leading to infective, painful deep ulcers. Such an area can be anywhere in the body that rests on a surface, or secured tightly by tubes and left for a period of time without being shifted across as considered ideal.
People with bed sores (pressure ulcers) can experience great pain, discomfort, depression and reduced quality of life. The aim of the attendant or carer should be to prevent, minimize and manage pressure sores. Here are some tips:
- Routine regular turning and repositioning of their loved ones in bed.
- Utilizing cotton to underlay and clothes that comes in direct contact with skin, this absorbs sweat and promotes skin breathe through.
- Use of bedding that is soft and non-plastic in nature.
- Use of moisture absorbent sheets to avoid the skin bathe in the body fluids.
- Encouraging time out of bed.
- Use of frames, slings or slide sheets to mobilize, rather than pull, push that can cause shearing force on the skin.
- Provide passive range of motion exercise regularly and encourage active movements of body as far as possible.
2. Pneumonia:
- Position in bed can be varying rather than supine or facing ceiling every time.
- Prone or semi prone position of lying will assist better aeration of lungs and also break from pressure areas.
- Head of the bed to be elevated at all times except when sleeping.
- Encourage deep breathing and coughing exercise as frequently as possible. Some of the other exercises can be blowing candles or light objects, blowing through straws into a half filled water bottle (Spirometry). This enables positive end-expiratory pressure (PEEP) and vibration to help in removal of secretion in the lungs that can cause pneumonia.
- Prompt pain relief of any source is very important for an individual to breathe adequately.
- Overt filling of stomach space or collections of fluid or gas in the stomach can cause back pressure to squash lung space.
- Enable normal forward passage of the contents of stomach, in some instances it could be active removal through nasogastric tubes.
- Offer frequent mouth care and frequent suction of the oropharynx or back of the mouth, as this can cause secondary issues such as aspiration that can also cause pneumonia.
3. Constipation:
- Offer regular food and fluids if not contraindicated as tolerated.
- Fluids to be warm
- Add roughage to diet if allowed and tolerated
- Regular toilet routine
- Use of fruits such as figs, prunes in diet
- Aperients as prescribed (a drug used to relieve constipation).
- Range of motion exercises and mobility in itself will assist with forward motion of bowel contents.
4. Contractures:
- Active and passive exercise will assist in prevention of contractures
- Use of appropriate support for the limbs while placed in any position
- Splints, wedges and materials rolled and packed for maintaining natural contour and shape of the body is essential
- Monitoring extremities for drop and lack of natural strength is important.
- Medications to assist with pain and relaxation can also aid in prevention of contractures.
- Provide comfort measures as required.
5. Deformity of Muscle and Joints
Resting in bed for long is deceptively thought to be healing in nature, but it is contradictory to what our body is designed for. One of the common concerns is deformity of muscle and joints due to stiffness. This not only leads to limitations in mobility, but also pain. The range of motion gets affected in the upper and lower limbs and joints, hampering independent feeding, hygiene, weight bearing and mobility. Commonly found deformities are: wrist and foot drops, both of which can be prevented to an extent. Preventive measures include exercises and use of devices that help maintain normal alignment of body parts.
Addressing Deformity and Stiffness
- A small towel or a roll of face washer can be given to hold in the palm.
- Frequent active and passive movements of the fingers and wrist joints.
- Stress balls, squishy material or toys can help in maintaining range of motions.
- Interlacing one’s own hands, making motions of wringing hands is another exercise one can try.
- Warm water baths (immersing hands into warm water baths) prior to active and passive range of motion can alleviate pain and improve restrictive movements.
- Legs resting in a slab and L shaped orthotic device can assist maintaining the normal shape of the feet.
- Wearing well-fitting clothes will relieve pressure that could impede circulation.
- Ensuring full range of motions of the joints, right from head to toe, to be encouraged as tolerated. This can be passive if not active.
6. Recurrent Urinary Tract Infection (UTI):
Stagnation of urine in the bladder, secondary to lack of neuronal supply can be a challenge.
- This requires manual emptying with in and out catheterization. This requires special skill.
- Frequent change of soiled underwear or diaper, will aid in prevention of ascending infection.
- Offer frequent generous amounts of fluids to keep system well flushed.
- Monitor for signs of infection.
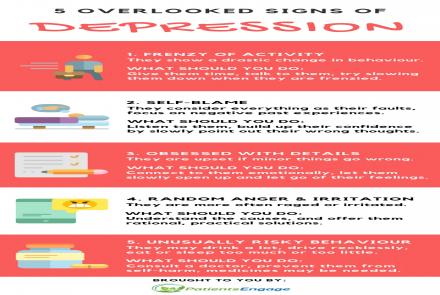
7. Depression
A bedridden patient can easily get depressed with a sense of incapacitation due to illness and disability. Or if confined within four walls, with a fixed view, dull lighting and minimal interaction. It is important to provide adequate routine to enhance comfort and relief from pain. Various therapies such as massage, hot water bath just prior to bed time, relaxation with aromatherapy, etc. can have deep impact in managing depression. Some useful tips
- Move the bed to a well-lit room, with good cross ventilation.
- Fulfil social and emotional needs. Fostering these through support service that includes sessions of music or meditation can assist alleviate some of the symptoms of depression.
- Playing calm, soothing music depending upon what your loved one likes. It could often be numbing for the caregiver, but the focus is your loved one here.
- Encourage communication, positive thinking and interactions that will enable them to ventilate their feelings. This will assist us in setting up their daily routine - whether that is a visit from the clergy, a friend, a video chat, a Skype session, an uplifting social meet, playing memorable videos, etc.
- Interior décor of the room can add to moods and feelings. It should be comfortable and aesthetically pleasing.

Born and schooled in India, Usha Ravi works in the area of critical care as an Advanced Nurse Practitioner (ANP) in Paediatric Critical Care in Australia. Supports community work at various levels. She truly believes clinical practice is her passion. In service for the last 24 years, she performs music to re-energize myself to embrace the everyday challenges. Together, with her husband and children and a very hyperactive working dog, they make a lovely home leaving her no time and reason to complain.