
Organ, tissue and cell transplants are sometimes the solution for certain conditions. This explains the basics of transplantation, types of transplants, lifespan of common transplanted organs and basic steps to preventing organ rejection.
What is Transplantation?
Transplantation is the procedure whereby an organ, tissue or cells is removed from one area of the body and implanted to another part of the body of the same or another person’s body. The tissue or organ is sometimes called “graft” or “transplant”. The person who provides the organ or tissue or cells is called the ‘donor’, while the one who receives them is called the ‘recipient’.
Examples of transplant include:
Organs- liver, kidney, pancreas, intestines, lung, heart, stomach, hands, limbs.
Tissues- skin, cornea, bone, heart valves, tendons.
Cells- hair, bone marrow, stem cells.
What should be known about a Transplant?
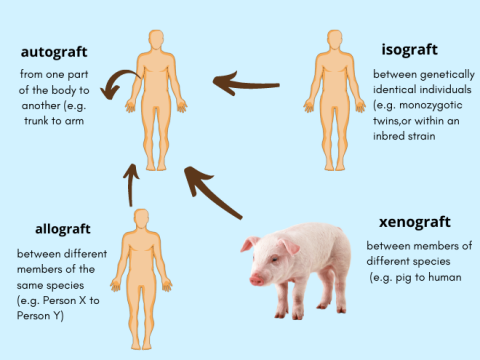
There are many types of transplants. The type of transplant carries out depends on several factors such as availability, compatibility, part of body etc. Let’s look at the common transplants:
- Autograft is where one part of the person’s body is implanted elsewhere in the same person. This is most recommended when possible and during emergencies. Examples include hair, skin, blood vessels, bone and bone marrow
- Allograft is where a part of a person is implanted into another person. Examples include kidney, heart, lungs.
- Isograft is when the transplant takes place between identical twins. The risk of rejection is the least in such transplants as the organ is genetically identical. Examples are bone marrow and kidney transplant
- Xenograft is when a part of an animal is implanted into a human. Pig organs are commonly used for heart valves, skin derma and kidney
Transplantation is a surgical procedure that must be carried by expert transplant surgeons. With advancing science, possibilities now include transplants of face and multiple organs. Common multi-organ transplants include heart with lungs or pancreas with kidney.
How do you know you need a transplant?
A person may require a transplant if they suffer from a genetic disease such as a heart defect, polycystic kidney disease, etc. Other reasons for an organ transplant would include damage to the organ by a chronic disease like diabetes, cirrhosis, pulmonary fibrosis, cancer etc, or from injury due to an accident or infections such as hepatitis.
Deteriorating organ function may be sudden or gradual depending on the causative factor. Your treating doctor will be monitoring your organ health via regular scans and blood tests. When the organ function starts to fail or if a transplant can improve your quality of life (by removing the need for dialysis, or oxygen support), you will be considered for transplantation.
Where do transplants come from?
A transplant or graft can come from a living or diseased person. Living donors are those who are compatible for donation and are often relatives. In case of dead donors, if there is brain death, the heart is sustained by machines to keep the organs viable till extraction. If the heart is dead, such as in cardiac arrest, then the extraction must be done speedily before the organ/tissue dies.
Nowadays, many parents choose to have their newborn’s umbilical cord cells harvested at the time of birth and freeze them in specialised storage facilities.
What happens before and after the surgery?
The process starts when you are identified to be a suitable candidate for transplant after a thorough assessment by your doctor and counselling session with a Transplant counsellor. You will then be put on the Transplant list or registry. When a donor has been found and matched, you will be notified and prepped for surgery. As organs do not survive for long outside a body, this process is expedited. Surgery often takes place in a few hours after a donor is found.
After the surgery, you will be monitored closely to see if the new transplant is working properly. You may spend significant time in the ICU and in a private room at the hospital. Special care is taken to prevent risk of any infection. Rehabilitation will also start as part of the recovery process with trained physiotherapists.
The recipient is additionally put on medications that will prevent their own immunity system from rejecting the new organ. These medications are called Immunosuppressants. They work by decreasing the immune system of the body. In doing so, the body is now vulnerable to microbes (bacteria, viruses, fungi etc.), and hence recipients must take added precautions to avoid all infections, even the common cold or flu.
Are there any side effects of Immunosuppressive medication?
The main side-effect of immunosuppressant drugs is the increased risk of acquiring infections. Specific side-effects will depend on the type of immunosuppressant. Make sure you read and understand all the side-effects before you start taking the medication, so you can watch out for symptoms. For instance, fever is a sign of infection and should be reported to your doctor right away. Do not stop taking your immunosuppressants unless advised by your doctor.
Types of immunosuppressant drugs used are:
- Calcineurin inhibitors (tacrolimus)
- Antiproliferative agents (mycophenolate mofetil)
- mTOR inhibitors (sirolimus)
- Corticosteroids (prednisone)
What are signs of organ rejection?
- The organ's function may start to decline.
- Flu-like symptoms, such as body pain, nausea, cough, chills and shortness of breath.
- General discomfort, uneasiness, or ill feeling.
- Pain or swelling in the area of the organ (rare)
- Fever (rare)
How to prevent organ rejection?
Here are a few ways to prevent infections. Transplant recipients should adopt these as lifestyle changes.
- Handwashing with soap and water is a simple and effective way to prevent infections. Wash your hands before and after eating, using the bathroom, cooking food, gardening, working outside or petting animals.
- Stay away from people who have active infections such as cold, flu, etc.
- Avoid coming in contact with animal faeces.
- Use mask and gloves as needed.
- Take your vaccinations on time and as advised.
- Avoid street and outside foods. Stick to homemade and hygienic meal preparations.
- Wash fruits and vegetables thoroughly before consuming.
- Stay active and exercise regularly.
- Avoid risks of getting any serious lifestyle illnesses like diabetes, obesity, hypertension etc.
- Sleep well and avoid stress.
How long does a transplant last?
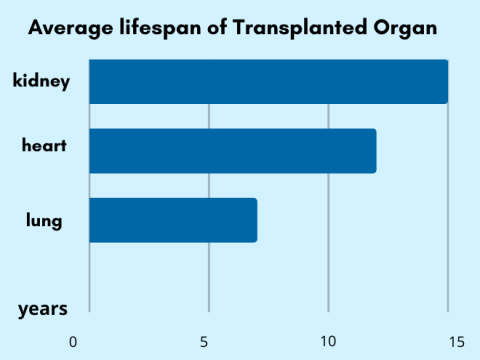
A transplanted organ life is calculated in terms of half-life. This is the point at which half of the organ has failed and the other is still functioning. This is not an accurate measurement because various factors can affect an organ’s life. However, it can provide a rough estimate of how long a transplanted organ may survive.
Kidneys (from living donors) are noted to be the longest surviving with a half-life of 21 years. A cadaver kidney has a half-life of about 9 years. Liver is also known to survive for very long as it has the capability to regenerate. The half-life of a lung is the shortest because it is exposed to many more environmental factors and infections.
Self-care, strict hygiene and adherence to the treatment plan can aid in the longer life of a transplanted organ.
References:
Health Resources & Service Administration: https://www.organdonor.gov/learn/process/transplant-process






