We know that stroke is a leading cause of disability. Dr. Nitin Sampat, Consulting Neurologist and Clinical Neurophysiologist highlights how stroke affects women differently, the risk factors for stroke in women and the preventive measures that can be taken.
In India, the incidence of stroke is 84-260 lakh annually and the stroke rate in people > 70 years is 1.5% per year.
It is the 4th leading cause of death and it still accounts for 1.3% of all causes of death in the world. However, it is the leading cause of disability & this may be permanent in a proportion of people.
Definition of stroke
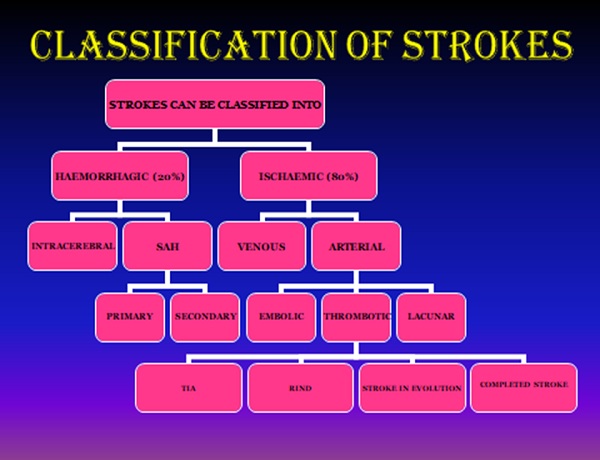
Strokes are a heterogenous group of disorders often resulting in sudden onset of development of a neurological deficit – (paralysis of hand and/or leg, facial deviation, slurring of speech, difficulty in talking or swallowing, double vision etc or permutation /combination thereof), linked by a common thread of occlusion (thromboembolic-ischemic) or rupture of cerebral blood vessels (haemorrhagic stroke)-- either arterial or venous.
Stroke in women
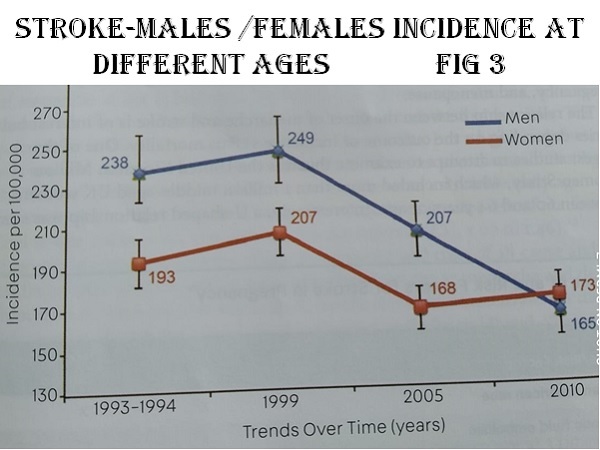
Stroke affects women differently than men because of their reproductive life and overall longer lifespan. Stroke incidence & prevalence is lower in females than in males though ethnic differences play a part. The onset of a stroke occurs 4 years later than in males but has a worse prognosis & a higher mortality rate.
The reproductive life span of a woman (age at menopause to age at menarche) < 30 years increases the probability of developing a stroke. Although the incidence of stroke in women is lesser than in men all through their life span, in later life, women have 1:5 risk while men have 1:6 risk of developing a stroke as incidence of stroke decreases in males but not in females.
Women over 80 years have a 13.4% prevalence while men have 11.5%. Between 60-79 years M:F is 6.5 : 5.4%.
Epidemiology
Although the non-reproductive risks of stroke overlap between men and women, those with greater impact on women include age, hypertension, atrial fibrillation, socioeconomic status & depression.
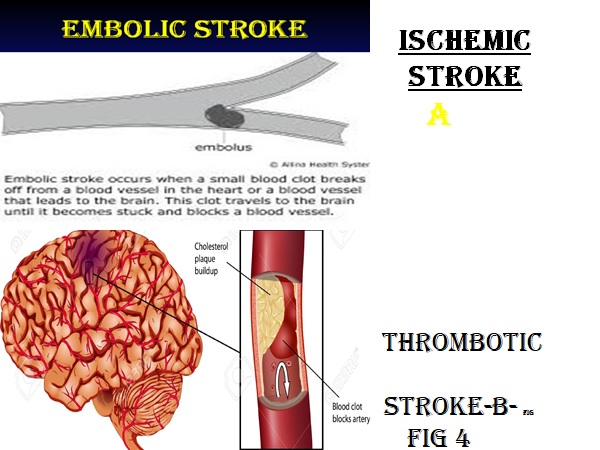
Ischemic strokes can be thrombotic or embolic from the heart or the carotid vessels in the neck
Signs & symptoms
Women present with non-traditional symptoms like headache, fatigue, disorientation, light-headedness, nausea, hiccups, change in vision & altered mental status. Ignoring these symptoms often leading to delay in the stroke diagnosis .
Risk factors
- Hypertension: Stroke producing potential of hypertension in both ischemic & haemorrhagic strokes, is a product of elevated systolic as well as diastolic pressure (Rabkin et al). Collins et al convincingly demonstrated that the long-term control of hypertension decreased the incidence of both ischemic & haemorrhagic strokes in women, compared to men. Women over 65 years of age, have a higher prevalence of hypertension & women with stroke are more likely to have hypertension probably due to later age of stroke onset.
- Atrial fibrillation (AF): In embolic strokes, risk factors are arrythmias especially atrial fibrillation which increases the incidence of stroke 6-fold. The presence of congestive cardiac failure, coronary atherosclerosis also enhances the stroke risk. AF has a higher impact on the risk of stroke in women due to more advanced age & women have a more severe stroke presentation than men in AF. Embolic strokes from the heart, often become haemorrhagic.
- Diabetic patients are twice as liable to strokes compared to age matched nondiabetics.
- Hyperlipidaemia especially high LDL cholesterol & high triglycerides contribute to the risk of stroke significantly. Use of lipid lowering drugs- statins, have been shown , by many clinical trials, to reduce stroke incidence considerably.
- Genetic risk factors & genetically determined diseases like sickle cell disease where the red blood cells contain an abnormal haemoglobin which is less soluble than normal Hb. In all individuals these sickled RBCs containing Hbs polymers are less deformable & there is a greatly increased risk of stroke especially in homozygous & sickle thalassemia genotypes. This may be predicted by documenting high velocity blood flow within the middle cerebral artery on the trans-cranial doppler test. Treatment is antibiotics, hydroxyurea, exchange transfusions & stem cell transplant. A new monoclonal antibody crizanlizumab (an anti-P selectin antibody) is now available to us as monotherapy or with hydroxyurea, it has revolutionised sickle cell therapy. In pregnancy sickle considerably increases the incidence of venous thrombosis.
In women, oral contraceptives, hormonal changes in different stages of reproductive life & of course, smoking (active smoking in pregnancy increases the risk of stroke 2-4 times), excessive alcohol, sleep apnea, prothrombotic or hypercoagulable states & vasculitis increase the likelihood of stroke.
These are modifiable risk factors (obesity & sedentary lifestyle included) but there are some non-modifiable risk factors like age, sex, race & family history. Asians develop atherosclerosis in intracranial more than extracranial blood vessels & African Americans develop more strokes than caucasians.
Related: Listen to neurologist Dr. Bhushan Joshi speak about Stroke and how it affects women, especially during Pregnancy
Pregnancy & stroke - Pregnancy & puerperium confer an increased risk with the incidence rates being 3-fold higher as compared to non-pregnant women. The highest risk is in the postpartum period coinciding with the highest risk of hypertensive disorders of pregnancy & peak gestational hypercoagulability.
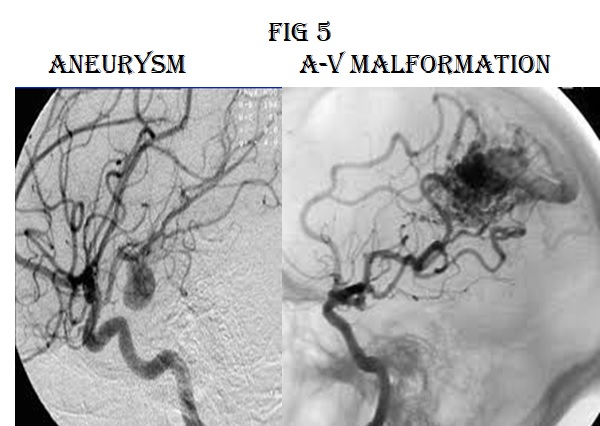
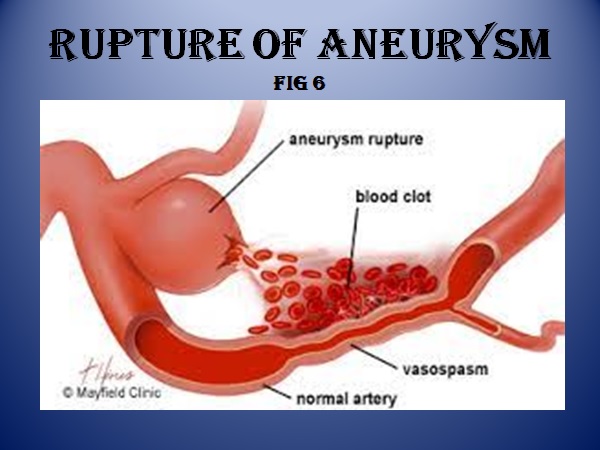
Bleeding from rupture of arterio-venous malformations & aneurysms do occur more at the time of delivery.
The rate of stroke remained unchanged from 1990 to 2017. Smoking is highly prevalent in women who develop strokes in pregnancy. In the US, this increase was seen in pre-eclampsia potentiated by posterior reversible encephalopathy--a syndrome of hypertensive encephalopathy characterized by reversible brain oedema.
Reversible Cerebral Vasoconstriction Syndrome (RCVS)-- shows segmental narrowing & dilatation of intracranial arteries. This too contributes to the causation of stroke in pregnancy but the outcome is favourable, only 5% having severe residual disability.
Other medical risk factors in pregnancy include genitourinary infection & sepsis & hormonally assisted reproductive therapies which increase ischemic stroke, probably by ovarian overstimulation & this activates the renin-angiotensin system with modification of sodium balance, BP regulation, and fluid shifts leading to hypercoagulability.
Risk of peripartum stroke is 34.3/100,000 births in women with caesarean as opposed to 7.1/100,000 with vaginal delivery. The increased risk in women undergoing caesarean delivery persisted up to 12 months post delivery.
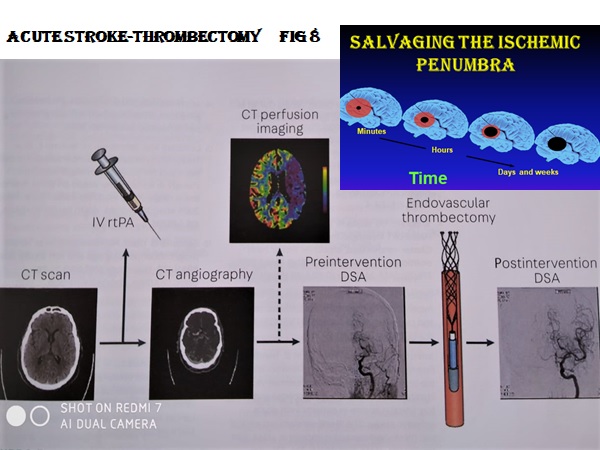
Pathophysiology of ischemic stroke - Initially due to loss of oxygen & glucose, as a result of a clot, the brain cells begin to die and are surrounded by live cells. This is called an ischemic penumbra where the dead cells can continue to die hence time is of essence.
Cerebral venous thrombosis - It is an uncommon cause of
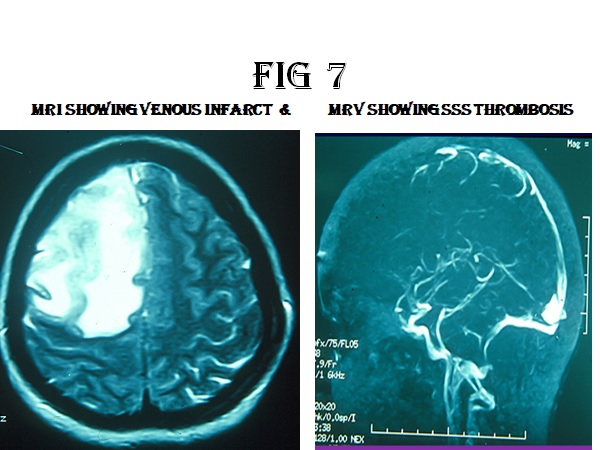
stroke and occurs more frequently in pregnancy & puerperium due to the hypercoagulable state, pre-existing in pregnancy. The recovery is fairly good in women with sex specific factors. It can be septic or aseptic. There is a triad of prothrombotic stage (34%), venous stasis & involvement of vessel wall.
Effort should be made to detect the prothrombotic factors & infections causing this state. Low molecular weight heparin even if there is a small haemorrhage, followed by new oral anticoagulants for a year or so depending on the underlying cause, if any.
Stroke outcomes - Women after strokes have worse outcomes than men as a result of older age at stroke onset, worse pre-stroke functional status & multiple co-morbidities including hormonal fluctuations.
Women who have had hypertensive disorders of pregnancy have 3.7% risk of developing new onset hypertension after 14 years of follow up than women who have not.
Oral Contraceptives - The risk of ischemic stroke is 1.7% higher in users than in non-users (2015 Cochrane review) especially if the contraceptives contain increased doses of oestrogen, but progestin-only contraception confers no increased risk of stroke. People on OC, who have prothrombin gene G 20210 mutation have a much greater chance of developing venous strokes.
Relation of menopause & stroke - Menopause is defined as absence of menstrual periods for at least 12 consecutive months. Oestrogen has a protective effect on vessels, this is lost in menopause occurring early i.e. before the age 40 years.
Vasomotor symptoms like hot flushes & night sweats, seen during menopause, had increased association of heart disease & stroke, as also risk factors like hypertension & hyperlipaemia. The interrelation of the autonomic nervous system & anxiety, depression & poor sleep, associated with menopause, have a higher risk of cerebrovascular disease.
Now hormone replacement therapy is used to reduce vasomotor symptoms but if given late (> 10 years after menopause), it increases the risk of thromboembolic events & this does not occur if given early after menopause especially by transdermal route.
Treatment is divided between a) acute ischemic stroke b) embolic stroke c) haemorrhagic stroke d)maintenance therapy e) secondary prevention f) rehabilitation
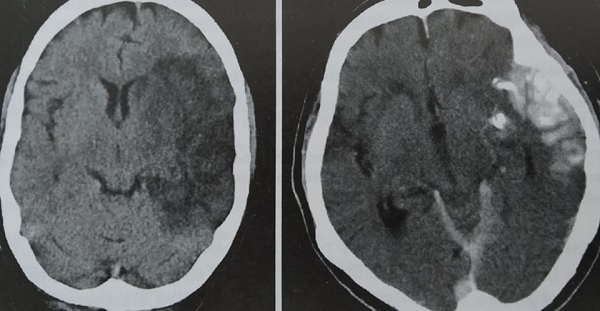
When a patient comes in within 4.5 hrs from onset of stroke (see fig 7), a CT scan is done. If there is no haemorrhage or any other contraindications, she should be thrombolysed after bringing down the BP. The revascularisation if done in time, irrespective of the age of the patient gives considerable recovery in 24 hrs & at 3 weeks. If recovery is limited or there is a major vessel occlusion or the patient comes after the stipulated 4.5 hours, thrombectomy is done.
In the acute phase, if thrombolysis is contraindicated aspirin can be used. Dual antiplatelets can be used for 90 days & then clopidogrel, which the Caprie trial showed was superior to aspirin in the brain or aggrenox is given. Newer antiplatelets like ticagrelor is fast acting, reversible & is more efficacious but in spite of the Thalis trial, a black box warning is issued by the US FDA, against its use in stokes, as the incidence of i-c bleeding is high.
Statins, Atorvastatin ideally 40-80mg is given to lower lipids to stabilise the plaques & reduce the growth of the thrombus. Many patients do not tolerate high doses of statins & get a lot of muscle pains, then lower doses are used.
If embolic infarcts are suspected warfarin or if AF is present new oral anticoagulants are used. Now antidotes are available against dabigatran, rivoraxoban, apixaban, these are equieffective as Vitamin K antagonists like warfarin, with much lesser chance of bleeding & less monitoring required. However, noacs are preferably avoided in pregnancy.
If the embolic source is stenosis
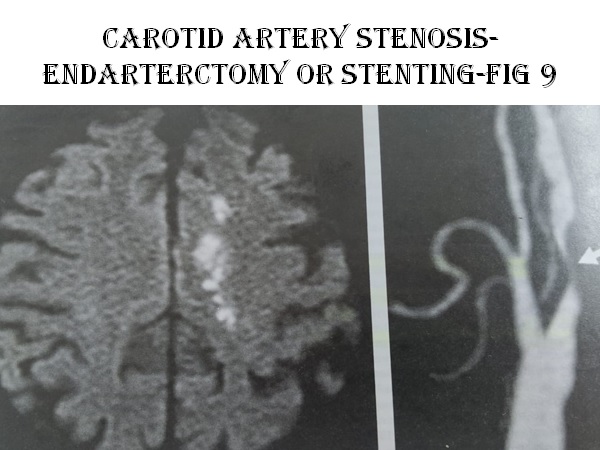
in the carotids & it is >60 obstruction on the symptomatic side, dual anti platelets are used till early endarterectomy or stenting is done
Puerperium was the period of highest risk of an obstetric ischemic stroke, the risk of recurrent stroke is not very high, but risk of miscarriages & foetal losses is high.
In haemorrhages cause should be determined with imaging, the BP should be gradually but adequately controlled, intracranial pressure reduced, seizures ,if any, controlled & supportive measures employed.
Rarely surgical intervention has to be done if all else fails. AVMs or aneurysms have to be tackled quickly surgically or by neuroradiological interventions to ward of the risk of rebleeding & probably death.
Early physiotherapy, mobilisation, rehabilitation, occupational therapy & speech therapy, where indicated, go a long way in helping stroke patients to return to a semblance of normalcy.
Secondary prevention of strokes
- Anti-platelets initially dual then clopidogrel in thrombotic strokes, anticoagulants like warfarin with an INR of 2-3 in cardioembolic strokes. Noacs if nonvalvular AF causing emboli.
- Statins to reduce cholesterol & to stabilise plaques. If LDL cholesterol not controlled ezetimibe or proprotein convertase subtilisin / kexin type 9 inhibitors may be added.
- Early detection & control of risk factors-BP~ 130/80, HbA1c between 6.5-7 , detection & control of high homocysteine , correction of Vit D deficiency, treat sleep apnoea by CPAP and manage all cardiac conditions.
- Stressful jobs, if present, should be helped by yoga or relaxation exercises.
- Depression- women have higher rates of depression which can lead to higher rates of poor health factors. Post stroke depression is seen in a proportion of patients more so in women. SSRIs like sertraline or escitalopram or SNRIs like venlaflaxine are useful along with yoga & psychotherapy, if indicated.
- Weight reduction if obese, physical activity reduces stroke in both men & women. 75 minutes of vigorous intensity activity per week is advocated.
Conclusion - Stroke is a devastating entity in view of the high mortality, but much more so due to the extensive disability, which could be permanent. Rapid strides have been made in the last two decades like thrombolysis ,thrombectomy, newer forms of rehabilitation & drugs. Still, we have a long way to go.
Take home message - Prevention is better than cure! This includes adequate early control of risk factors, early detection of the unusual presentations in women, handling the aetiologies during the reproductive years, and prompt reporting to stroke units for thrombolysis!
References
- Continuum :- Cerebrovascular disease April 2020
- Neurologic clinics:- Neurology of pregnancy Feb 2019
- Stroke:-pathophysiology diagnosis and management Elsevier 2011
- The lancet neurology :- Jan 2021
- Cerebrovascular disease: controversies and challenges –Neurologic clinics May 2015
- Neurology:- Jan 2021
- International journal of stroke:- Stroke incidence prevalence & mortality in women worldwide 2016
- Pregnancy & neurologic disease:- Neurologic clinics aug 2012
- Bradley’s neurology in clinical practice vol 2 Elsevier-seventh ed 2016
- Jama neurology 2016:- risk factors for stroke a schematic review & meta analysis
- Lancet:- Global health 2018
- Conns current therapy 2020 Elsevier
- Swaimans paediatric neurology fifth ed. Elsevier
Diagrams provided by Dr. Sampat
Dr Nitin Sampat:
Qualifications: MBBS; MCPS; MD (Gen. Med.) Dip. NBE (neuro)
Consulting neurologist & clinical neurophysiologist with Bhatia General, Wockhardt and Global hospital in Mumbai. Practicing since 38 years with special interest in stroke/headache/ epilepsy/clinical electrophysiology and sleep disorders.
Memberships
o American academy of neurology
o International headache society
o World federation of neurology
o Neurological society of India
o Indian academy of neurology