People often have to deal with pain and it is difficult to assess the level of pain across different people. Pallium India has created the Indian Primer of Palliative Care for care providers. With their permission we have excerpted important elements that are useful to understand and manage pain.
Many people with chronic diseases will complain of pain and it being the most overpowering symptom of their condition. Besides physical discomfort, pain affects mental and emotional wellbeing thus potentially leading to debilitation of overall quality of life. In cancer, for example, 20-50% of the patients have pain and in advanced stages nearly 80% of patients suffer from moderate to severe pain.
The Indian Primer of Palliative Care manual generated by Pallium India puts forth a step-by-step guide on how as a care provider, one should go about acknowledging, assessing and providing options for management of pain for patients. Here are the key excerpts from the manual that are relevant for patients and their primary caregivers.
What is Pain?
According to the International Association for Study of Pain (IASP), pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage. Pain is not just a sensation or information appraisal but an emotional experience, so when a patient says it hurts, believe him or her.
Types of pain
There are several ways to categorize pain. One way is to separate it based on duration of the pain. This includes:
- Acute pain is that which is brought on suddenly but is short lasting. It indicates tissue injury and responds well to treatment.
- Chronic pain is that which is long-lasting and likely to include nerve damage as well. It is unremitting and often progressive as it takes on the characteristics of the disease itself.
Both acute and chronic pain can psychologically affect the patient leading to depression and anxiety. This is a vicious circle as psychological factors can further aggravate the pain. If the pain originates from a psychological disorder, it is termed Psychogenic Pain. Pain can also be classified by the causative factor. This includes:
- Nociceptive pain is when pain arises from tissues and is reported to the brain. This includes nausea, tumours, inflammation etc.
- Neuropathic pain is when the pain arises from the nervous system itself. This includes injury, damage or pinching of nerves due to chemotherapy, spinal metastasis, alcoholism, phantom limb pain etc.
The types of pain can overlap in situations where both tissue and nerve damage is seen.
Pain assessment
Always listen carefully to the patient regarding his/her pain. Pain can be particular to each patient. Always evaluate how is the pain affecting the person and what impact it has? The meaning that the patient may attribute to the suffering is very significant. It is important to know the patient’s understanding of the cause and reason for the pain. All of this needs to be acknowledged and addressed within the therapeutic plan. So conveying this information to your doctor is imperative. Ask about:
- Palliative as well as provocative factors if any.
- Quality of pain (nature of pain; e.g. burning, aching etc.).
- Radiation of pain to other parts of the body.
- Site and Severity.
- Temporal factors (duration, diurnal variation of pain, continuous or intermittent).
Pain scale
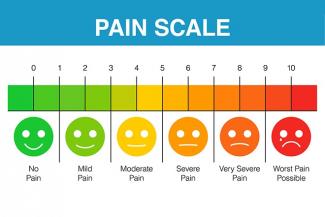
Various scales are available to help assess and rate the pain. The aim of pain management is to keep the pain score at a level that the patient considers satisfactory.
- Categorical Pain Scale: Patient is asked to grade his pain as having “no pain, mild pain, moderate pain, severe and excruciating pain.
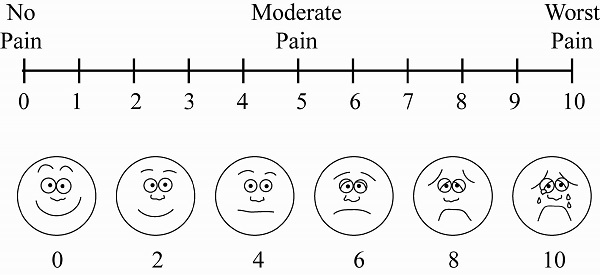
- Numerical Rating Scale (NRS):
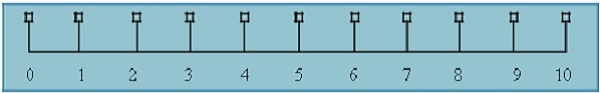
It is explained to the patient that zero represents “no pain” and 10 represents the “worst imaginable pain”. Then, the patient is asked to score his pain on this scale according to the severity. - Visual Analogue Scale (VAS) is usually used to assess pain in children.
The Analgesic ladder was developed by the World Health Organization (WHO) to create a 3 step approach for drug administration for cancer pain relief in adult patients. When pain occurs, the order (as seen in the image below) must be followed from the bottom going towards the top. Patients are started on non-opioid drugs such as aspirin or paracetamol, then if required moved to a mild opioid like codeine; then stronger opioid such as morphine till patient is pain free. Adjuvant drugs are used to alleviate additional symptoms.
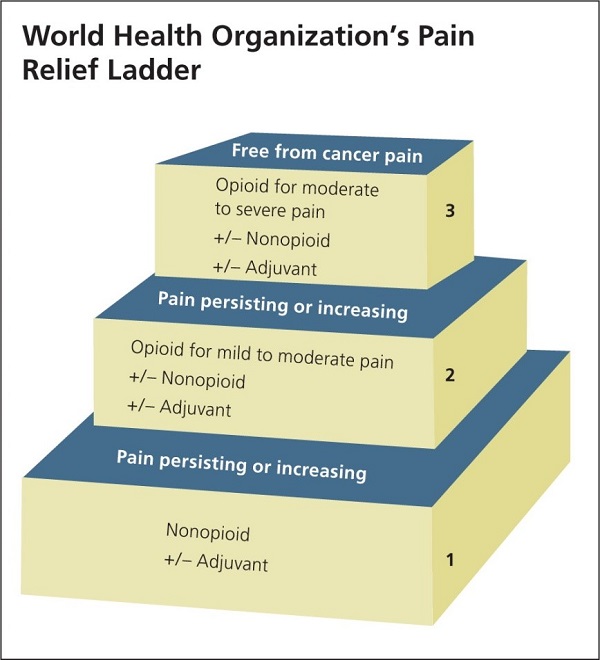
WHO recommendations for Pain relief:
- Continuous pain needs continuous relief. Drugs should be given clock-wise every 3-6 hours and not on demand.
- Give medicines orally as much as possible. This is the simplest route. A well-informed patient can use the oral medications by himself. Injections require professional help, are sources of pain by themselves, and are best avoided.
- Medications can start at step 3 if pain is severe.
- If drugs are not effective, surgical intervention must be applied for further relief.
- Each person should be assessed in detail physically and holistically and managed accordingly.
- In children, a 2 step ladder is used.
Commonly used drugs in pain relief
|
Non-Opioids |
Opioids for mild to Moderate pain |
Opioids for moderate to severe pain |
Adjuvant analgesics |
|
Paracetamol |
Codeine |
Morphine |
Antidepressants |
Interventional techniques for pain
Interventional pain management involves pain blocking via minimally invasive methods. These include trigger point injections, nerve blocks, autonomic or sympathetic plexus blocks, and minimally invasive spinal interventional techniques (ablation of targeted nerves, intrathecal infusion pumps or spinal cord stimulators).
Interventional techniques are possible options for patients with failed oral or transdermal analgesic therapy and helps actively restore quality of life.
Non-drug options for pain relief:
- Empathy, counseling and psychotherapy are essential to address the subjective emotional component of the pain experience.
- Physical therapies such as heat, transcutaneous electrical nerve stimulation (TENS), ultrasound and exercise.
- Injection of trigger points with local anaesthetic agent.
- Modification of the patient’s living environment and use of assistive devices (ramps, toilet risers, walkers, wheelchairs etc.).
- Complimentary therapies including yoga, acupuncture and cognitive behavioral therapy (CBT) in improving pain-related behavior and perceived self-efficacy.
- Involvement in activities that bring joy to the individual’s daily life helps in moving beyond the constant presence that pain has in a person’s life.
Citations:
- Rajagopal MR, Vallath N, Mathews L, Rajashree KC. Watson M (ed). An Indian Primer of Palliative Care. 2017.
- International Association for Study of Pain (IASP) https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698
- NIH National Cancer Institute https://www.cancer.gov/about-cancer/treatment/side-effects/pain/pain-hp-pdq






