Treatment of oral cancer involves surgery, radiotherapy, chemotherapy, targeted therapy or immunotherapy. Treatment plan is decided based on severity, stage of the cancer and patient’s condition. Doctors may recommend some of the following:
1. Surgery – Surgical treatment is planned based on size, stage of cancer and patient’s condition.
- Tumor excision - It is done to remove the tumour and surrounding healthy tissue margins to ensure complete destruction of cancer cells. Excision depends on the size and location of the tumour.
- Neck dissection and removal of lymph nodes are done if it has spread into lymph nodes. This will prevent further spread of the cancer. Types of neck dissection include selective, modified radical, or radical neck dissection.
- Reconstruction surgery - It is performed to restore functions and aesthetic for improving quality of life of the patient. It involves flap reconstruction, skin grafting or the use of implants. If jaw bone is affected in advanced cancer, jaw is reconstructed with the help of bone grafting. In case of tongue involvement, reconstructive surgery is done to preserve speech and swallowing functions.
- Microvascular surgeries are performed to transplant tissue from another part of the body to reconstruct the affected area.
- After surgery, medicine and liquid nutrition support is given through a tube inserted from nose to stomach. Semi solid food can be given to patient after sutures have healed.
- Nutritional support and physiotherapy, rehabilitation services including swallow and, speech therapy help patients to regain optimal function after surgery.
2. Radiotherapy – It plays an important role in cancer therapy as definitive treatment or an adjuvant therapy. It kills cancer cells and stops them from multiplying. It is given through high energy beams of radiation directed towards the cancerous tissue. Radiotherapy is given in multiple sessions over months to allow healthy tissue to recover. It is recommended after surgery in patients who have high chance of the cancer recurring.
Side effects of radiation include dryness of mouth, ulcers, hair loss, dental cavities etc.
- Mucositis – Inflammation and ulceration of the oral mucosa.
- Xerostomia – Dryness of mouth is the common side effect of radiation. It leads to difficulty in eating, oral infection and dental caries.
- Dysphagia – Difficulty in swallowing happens due to inner inflammation of the throat and oesophageal tissues.
- Radiation dermatitis – Skin reactions such as redness, dryness and peeling can happen in the treatment area.
- Osteoradionecrosis, reduced mouth opening and radiation induced fibrosis are long term side effects of radiation.
3. Chemotherapy - Combinations of various drugs are used to slow down the cancer cell progress and kill the cancer cells. They damage DNA of cancer cells and kill them. Chemotherapy drugs are given orally and intravenously. Sometimes it is indicated before surgery to shrink tumour and east surgical resection. It can be used as the primary treatment modality for advanced or unresectable oral cancers, either alone or in combination with radiation therapy (chemo radiotherapy).
Common side effects include hair loss, fatigue, hematologic toxicity, neurotoxicity, nausea, vomiting and anaemia. For managing side effects of chemotherapy:
https://www.patientsengage.com/conditions/managing-side-effects-chemoth…
4. Targeted therapy - These are aimed at the altered cells due to cancer. It is used in cases where cancer has genetic mutations or resistant to other treatment. The molecules involved in cancer growth and progression are specifically targeted in this therapy. Commonly used drugs are cetuximab or pembrolizumab.
5. Immunotherapy – These are used alone or in combination with other treatments for advanced or recurrent oral cancer. It boosts the body’s immune system to recognize cancer cells, control the progression and kill them. Nivolumab and pembrolizumab are commonly used for oral cancer.
Read more on managing complications at
https://www.patientsengage.com/conditions/managing-oral-complications-c…
Go through some personal voices for motivation:
- https://www.youtube.com/watch?v=RzQewDzDRNc
- https://www.patientsengage.com/personal-voices/i-did-it-i-finally-quit-…
- https://www.patientsengage.com/personal-voices/oral-cancer-chewing-soli…
- https://www.patientsengage.com/personal-voices/ways-de-stress-during-ch…
References:
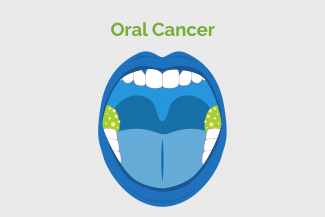
- Image 1 https://www.healthline.com/health/oral-cancer/oral-cancer-screening
- Image 2 and 3 - https://www.aafp.org/pubs/afp/issues/2002/0401/p1379.html
- https://www.ncbi.nlm.nih.gov/books/NBK343649/#:~:text=Oral%20cancer%20s…
- https://www.mayoclinic.org/diseases-conditions/mouth-cancer/diagnosis-t….
- https://www.nhs.uk/conditions/mouth-cancer/treatment/
- https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cance…
- https://www.cancer.org/cancer/types/oral-cavity-and-oropharyngeal-cance…(,tumors%20or%20slow%20their%20growth.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3170277/