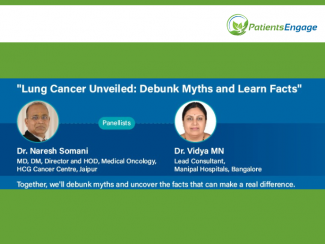
Dr. Naresh Somani ( MD,DM, Director and HoD Medical Oncology, HCG Cancer Centre Jaipur) & Dr. Vidya MN ( Lead Consultant, Pathology, Manipal Hospitals, Bangalore) spoke to PatientsEngage on myths and facts on lung cancer.
-
Myth: Lung cancer is just a chronic cough that will eventually go away.
Fact: Lung cancer is not merely a chronic cough that will disappear over time. While a persistent cough can be a symptom of various respiratory issues, including lung cancer, it is crucial not to dismiss it as a passing irritation. If a cough persists for more than two to three weeks, especially in individuals over 40 with a history of chronic smoking, it could indicate an underlying pathology such as lung cancer. Other symptoms to watch out for include blood-tinged sputum, chest pain, shortness of breath, unexplained weight loss, hoarseness, or changes in voice. Ignoring such symptoms could delay diagnosis and treatment, potentially allowing the cancer to progress. It's essential to seek medical attention promptly for proper evaluation and diagnosis. Diagnostic tests such as chest X-rays and CT scans may be needed to properly evaluate any suspicious findings, especially in individuals at high risk, such as chronic smokers. Early detection through proper investigation can significantly improve outcomes and treatment options for lung cancer.
-
Myth: Lung cancer only affects smokers.
Fact: It's incorrect to assume that only smokers are susceptible to lung cancer. In recent years, there has been a notable increase in lung cancer cases among non-smokers, particularly among women. This rise in incidence can be attributed to factors such as passive smoking (exposure to secondhand smoke), air pollution, and indoor pollutants like wood fuel or coal tar burning. While smoking remains a significant contributor to lung cancer cases, it's crucial to recognize that non-smokers across various age groups are also being diagnosed with this disease.
-
Myth: There's no point in quitting smoking after years of smoking because the damage is already done.
Fact: It's a misconception to believe that quitting smoking later on has no benefit. Regardless of the duration of smoking, quitting smoking significantly reduces the risk of various health issues, including cancer, heart disease, asthma, COPD, and brain damage. Within just 24 hours of quitting, the body starts to repair itself, and the risk of developing heart disease and experiencing a stroke begins to decrease. The idea that the risk diminishes to zero after quitting for a certain period is false; the risk remains elevated compared to non-smokers. Smoking cessation is always beneficial, and there's no concept of "safe" or "low-risk" smoking. Additionally, smoking not only causes lung cancer but also increases the risk of various other cancers, such as gastrointestinal, pancreatic, and bladder cancers. Therefore, it's crucial for individuals to understand the broad spectrum of health risks associated with smoking and make informed decisions to quit smoking for their overall well-being.
-
Myth: E-cigarettes or vaping is safer than traditional smoking and does not cause lung cancer.
Fact: There is currently no direct evidence linking vaping to lung cancer. However, it's essential to recognize that lung cancer typically develops after many years of exposure to toxins. Vaping is a relatively new phenomenon, and the long-term effects on lung health are still unknown. It will require ongoing research over the coming years to determine if there is an association between vaping and lung cancer or other lung diseases. It's also crucial to understand that vaping may serve as a gateway to traditional smoking, as many individuals who start with e-cigarettes eventually transition to tobacco or nicotine smoking, which poses significant health risks. Therefore, while vaping may seem less harmful initially, it's essential to exercise caution and be mindful of potential long-term consequences.
-
Myth: Once diagnosed with lung cancer, there's no reason to quit smoking, as the damage is already done.
Fact: Continuing to smoke during active cancer treatment, such as chemotherapy, can lead to inferior results and poorer outcomes. Moreover, if surgery is a possibility, smoking increases the risk of complications. It's a misconception that smoking has no impact once treatment has started. In reality, quitting smoking can enhance the effectiveness of chemotherapy and improve the chances of recovery. It's important for individuals to understand that smoking cessation significantly influences treatment outcomes and overall prognosis, even after a cancer diagnosis.
-
Myth: Air pollution does not cause lung cancer; it's just a myth.
Fact: Air pollution, especially in larger cities, has been directly linked to lung cancer. Prolonged exposure to pollutants, such as carbon particles, can lead to inflammation in the lungs and increase the risk of cancer over time. This is particularly concerning in urban areas where residents are chronically exposed to high levels of pollution. The recent focus on air quality in cities like New Delhi underscores the severity of the issue. While individuals may feel helpless against high pollution levels, it's essential to advocate for strong policies and collective action to address this problem. Community participation is crucial in reducing air pollution levels and ultimately lowering the incidence of lung cancer. It's not just limited to metropolitan areas; even smaller towns and industrial townships are experiencing alarming levels of pollution, affecting both smokers and non-smokers alike. Furthermore, the rise in adenocarcinoma, a type of lung cancer commonly seen in non-smokers and younger individuals, underscores the need for increased awareness and vigilance across all demographics.
-
Myth: The series of tests conducted during the diagnosis of lung cancer are unnecessary and delay treatment.
Fact: The process of diagnosing lung cancer involves several tests for a reason. While it may seem lengthy to patients, each step is crucial for accurately understanding the nature of the cancer and determining the most effective treatment plan. In particular, for non-small cell lung cancer (NSCLC), molecular testing using platforms like NGS (Next-Generation Sequencing) is essential. These tests analyze genetic mutations and predict the tumor's response to targeted therapies and immunotherapy drugs. It's important for patients and their families to grasp that these tests are integral to personalized treatment strategies, not just for advanced lung cancer but also for stages two and three. Therefore, undergoing comprehensive testing ensures that patients receive the most appropriate and effective treatments for their specific type of lung cancer.
-
Myth: In the past, it was believed that stage four lung cancer is untreatable with low survival rates.
Fact: This perception is now a myth. The outcomes for stage four lung cancer patients, whether they have actionable mutations or not, have significantly improved. With advancements in treatments based on NGS mutation detection and combinations of immunotherapy with or without chemotherapy, patients now have a 60-70% chance of responding to treatment. Survival rates have increased, and many patients are able to survive beyond two years. This marks a significant improvement in the overall prognosis for stage four lung cancer patients.
-
Myth: All lung cancers receive the same treatment, and patients are often surprised when they discover that their treatments differ from others.
Fact: Lung cancer treatment is highly personalized, tailored to each patient's specific type of cancer and genetic mutations present in the tumor. Small cell lung cancer and non-small cell lung cancer (NSCLC) are treated differently, with NSCLC further divided into subtypes like squamous cell carcinoma and adenocarcinoma. Genetic testing, such as Next-Generation Sequencing (NGS) and PD-L1 testing, helps identify actionable mutations that influence treatment decisions. Adenocarcinoma, particularly in Asian or Indian populations, often presents actionable mutations, while squamous cell carcinoma typically lacks actionable mutations. Treatment plans may include chemotherapy, immunotherapy, targeted therapies, or a combination, depending on individual factors. This personalized approach, known as Precision Therapeutics, ensures that patients receive the most effective treatments for their unique circumstances, improving their chances of successful outcomes. Therefore, variations in treatments between patients are based on their specific genetic profiles and disease characteristics, rather than a one-size-fits-all approach.
-
Myth: "I have no family history of lung cancer, so I am safe."
Fact: While lung cancer is not typically a familial disease, it is primarily linked to environmental factors such as smoking, asbestos exposure, and pollution. Family history of lung cancer is rare, accounting for a very small percentage of cases. However, the shared behavior of smoking within families can contribute to an increased risk among relatives. Smoking itself becomes a familial risk factor, rather than a direct genetic inheritance of lung cancer.
-
Myth: "My wife was diagnosed with lung cancer, but then the doctor called it metastatic breast cancer. I'm confused."
Fact: When cancer reaches stage 4 and spreads to other parts of the body, it commonly affects specific organs like the brain, lungs, liver, and bones. Sometimes, the symptoms of metastasis can mimic those of the primary cancer, leading to initial confusion. However, thorough investigation, including biopsy and advanced imaging tests, helps identify the primary cancer site. In some cases, cancers initially diagnosed in one organ, such as the lung, may actually be metastases from cancers originating elsewhere, such as the breast. Successful treatment of the primary cancer doesn't guarantee immunity from metastasis, which often targets organs like the liver and lungs.
-
What are the different types of lung cancer?
When a pathologist diagnoses lung cancer, they typically categorize it as either non-small cell carcinoma or small cell carcinoma. Non-small cell carcinoma is further divided into subtypes such as adenocarcinoma and squamous cell carcinoma, which are the most common. Adenocarcinoma is often found in non-smokers, while squamous cell carcinoma is linked to smoking. Small cell carcinoma is less common but more aggressive, usually associated with smoking. These distinctions are important for determining the most effective treatment options, as each subtype may respond differently to treatment.
-
What do terms like "precision medicine" and "personalized medicine" mean in the context of cancer treatment, and how do they differ from immunotherapy?
Precision medicine and personalized medicine refer to the practice of tailoring cancer treatment to the specific genetic characteristics of each patient's tumor. This involves genetic testing, such as Next-Generation Sequencing (NGS), to identify mutations in the tumor. Patients with specific mutations receive targeted drugs designed to block the effects of those mutations, leading to more effective treatment with fewer side effects. On the other hand, immunotherapy harnesses the body's immune system to fight cancer cells. Rather than attacking the tumor directly, immunotherapy boosts the immune response, enabling the body to recognize and destroy cancer cells. Both approaches represent significant advancements in cancer treatment, offering more effective and less toxic options for patients
-
How are cellular differences between lung cancer and metastatic breast cancer determined, particularly through radiology?
When biopsies for lung cancer are received, one of the first steps is to review the radiology reports to understand the tumor's characteristics. Metastatic cancers are often presented as multiple tumors or with a characteristic 'Cannonball' appearance on imaging scans. However, if the clinical presentation and imaging suggest primary lung cancer, further analysis is proceeded with cautiously. Adenocarcinomas from various organs can appear similar under the microscope, so immunohistochemistry is employed to differentiate them. For instance, if a patient has a known history of breast cancer, breast-specific markers are used to ascertain if the lung tumor is indeed metastatic from the breast. This approach helps in distinguishing between primary lung cancer and metastases from other sites. While morphology can sometimes provide clues, immunohistochemistry plays a pivotal role, particularly in challenging cases where an accurate diagnosis is imperative.
-
Navigating Vaping Concerns and Treatment Decisions for lung cancer
It's understandable to have concerns about the long-term effects of vaping. Instead of turning to alternative methods that may lead to further addiction, it's advisable to focus on quitting smoking altogether. When seeking medical advice, it's crucial to listen to your healthcare team, including pulmonologists, radiologists, medical oncologists, and pathologists. Tests and treatments are recommended for a reason, and delaying them could impact your health outcomes. For lung cancer diagnosis, Next-Generation Sequencing (NGS) is increasingly important, so ensure you undergo this test if diagnosed with adenocarcinoma. Avoid unnecessary delays and prioritize timely diagnosis and treatment for better outcomes.
Closing remarks -
"Considering the uncertain long-term effects of vaping, it's best to prioritize quitting smoking entirely. Trust your medical team's advice during diagnosis and treatment, including recommended tests like NGS for lung cancer, for better outcomes."- Dr. Vidya
"Quit smoking for your health, your family, and our nation." – Dr Naresh Somani
“It's vital for people to realize why we're having this conversation. Understanding the importance of these tests is key. Merely going to the hospital doesn't mean tests are administered arbitrarily. Each test serves a purpose, shaping the treatment path and its success rate.” – Aparna Mittal






