
Varicose veins affects more than 1 in 5 persons. Dr Shital Raval explains what varicose veins are, the causes and risk factors, the tests for diagnosis, the treatment and self management for varicose veins.
What are varicose veins?
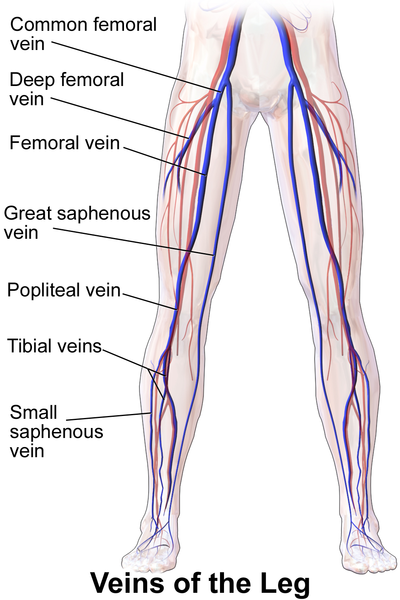
The venous system of the leg consists of 3 types of veins:
1. Superficial: long and short saphenous veins. These are principal veins near the surface of the legs.
2. Deep: veins that supply the muscles of the leg
3. Perforators: veins that connect the deep to the superficial veins
हिंदी में पढ़ें: वेरिकोज़ वेंस (अपस्फीत शिरा) के प्रबंधन के बारे में आवश्यक जानकारी
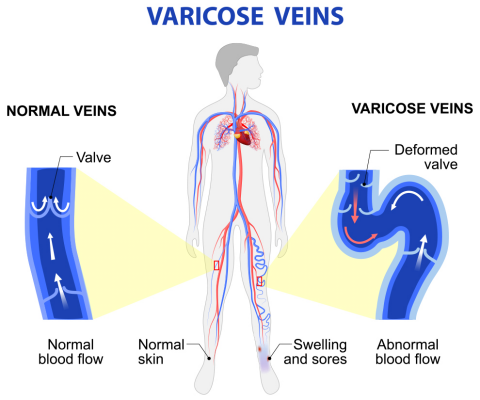
Almost all the veins, especially the larger ones have valves. Varicose veins are elongated, dilated, often tortuous veins that have incompetent valves.
According to the UK health authorities, up to 30% of adults are affected by varicose veins. But women are more at risk. The National Institutes of Health estimate that 33% of women and 17% of men in the US are affected.
What causes varicose veins
Normally, valves in the veins keep the blood flowing up towards the heart, so the blood does not stagnate in any place. But sometimes, the valves become defective and are unable to allow the blood to flow up. The blood accumulates in the veins, the veins swell up and pressure increases. The veins then become weaker, enlarged and twisted. They appear blue or dark purple in colour and cause pain and discomfort.
Some people develop spider veins. These are a milder form of varicose veins that occur just under the surface of the skin - around the face or leg. These appear as a ‘spider web’. They are not considered true varicose veins and are not a serious medical problem.
Are you at risk of developing varicose veins?
Risk factors include:
Gender: Women seem twice as susceptible to this condition, possibly due to the effect of progesterone on the venous system. Progesterone seems to weaken the walls of the veins and cause the veins to collect blood easily.
Age: The likelihood of developing varicose veins go up after the age of 30 as the elasticity of the veins weaken
Obesity: Increase in body weight increases the pressure on the veins of the legs and can gradually cause the valves to become incompetent
Family history: There is a hereditary component to this condition but the exact factors are not yet identified.
Pregnancy: Expectant mothers are most often seen to be affected by varicose veins due to pregnancy hormones, increased blood volume and pelvic pressure by the growing womb on the veins. Usually the veins return to normal a year after the delivery of the child.
Smoking: This causes low blood pressure in the venous system. Chronic smokers often have lower BP because the longterm effect of nicotine decreases appetite and weight, deposits chemicals in the blood vessel, increases risk of clots and slows blood flow
Certain kinds of jobs: Those that include a lot of standing are believed to cause varicose veins
Symptoms and signs of varicose veins
- Pain and heaviness while standing or sitting for a long time
- Burning sensation in the veins
- Purple or blue discoloration of veins
- Veins appear swollen and bulging like cords
- Itching around the veins
- Nocturnal (at night time) cramps
- In severe cases, ulcers may form around the ankle
You should consult a doctor as soon as you develop varicose veins, even if they are not painful, so you make sure they do not get worse.
How are varicose veins diagnosed?
Your doctor may suggest some of the following:
General examination to check for signs of venous insufficiency
Tests may include the following:
- Standing cough impulse test to check for reflux of the blood at the saphenofemoral junction
- Tap test - done while tapping the vein proximally
- Schwatze test to check the impulse on the saphenofemoral junction.
- Brodie-Trendelenburg test to determine competency of the veins
- Hand-held or colour Doppler, an ultrasound procedure to assess blood flow and structure of veins.
- Magnetic Resonance Venography (MRV), which shows a detailed map of the veins to find the possible cause of the condition.
Treatment options
Complications, although rare, can include thrombophlebitis (inflammation of the veins), deep vein thrombosis or blood clots, skin ulcers/eczema or lipodermatosclerosis(thickened fat layer under the skin). Rarely varicose vein may bleed! Hence treatment is a necessity to stop further complications.
Treatment options include self-care and compression stockings. For severe varicosity, surgical methods are used. These may include sclerotherapy, laser surgery, vein stripping, ambulatory phlebectomy or an endoscopic procedure. Be aware that some of these are considered cosmetic surgeries and that varicose veins may recur.
Self care essentials:
Compression stocking: These are tight fitted stockings that help compress the legs and prevent the back flow of the blood. These are very effective if worn daily and can even prevent and help heal any skin sores.
Reduce weight and eat a low-salt diet: Reducing weight decreases the strain on the veins and a low-salt diet helps decrease blood pressure.
Elevate legs: Patients are advised to raise and rest the legs above the heart level 3-4 times a day. This helps reduce swelling and relieve the pain and other symptoms.
Avoid standing or sitting for long and crossing legs while sitting.
Wear appropriate shoes: Avoid high heels or uncomfortable shoes.
Daily exercise: Some form of exercise helps circulate the blood and keeps the body healthier. Exercise increases the return of the blood flow to the heart and can help decrease the pain and occurrence of new varicose veins. Remember that the exercises must be performed gently and if there is any discomfort or pain, stop right away.
Exercises such as walking, running, pedaling on a stationary bike, swimming are most effective.
You can try these exercises as well:
(Please be advised to check with your doctor is its ok to do these or any other such exercises you come across or someone suggests)
1. While lying on your back, lift both the legs up and hold till the veins seem to drain out. Bring the legs down for a few minutes and repeat again for 20-30 minutes. This helps the flow of blood to the heart and decrease the pain and swelling.
2. While lying on your back, lift one leg up and bend the other. Rotate the legs as if riding a bicycle. Continue for at least 30 minutes daily (with breaks if needed). This will increase the blood circulation in the legs.
3. Stand while holding on to a bar for support. Raise the calf muscle by standing on your toes to stretch them. Repeat this several times till the calf muscles feel well stretched.
4. Lie on your back and gently bring one knee towards the chest. Now point, flex and rotate your ankle in all directions. This helps to tighten the calf muscles and tendons around the ankle. Repeat with the other leg.
Exercises such as strenuous weight-lifting, sitting for long periods as in yoga, sit-ups, crunches, lunges etc should be avoided as these can cause the blood to pool in the vein by impeding return.






