Specialty palliative care, in contrast to standard oncology care, can provide an extra layer of support for patients with lung cancer and their families. Dr Rajam Iyer, a pulmonologist and strong proponent of palliative care, enumerates its benefits for lung cancer patients.
What is palliative care for lung cancer?
In India, lung cancer constitutes 6.9 per cent of all new cancer cases and 9.3 per cent of all cancer related deaths in both sexes. At the time of diagnosis, almost 60% of patients with lung cancer are not eligible for radical treatment. Soothing and supportive treatment is a treatment of choice. Currently, palliative inpatient and home care are used for patients who present symptoms of constant, severe breathlessness at rest, chronic coughing, severe pain, muscle wasting and fatigue, anxiety and depression as well as significantly reduced physical and intellectual activities.
Most patients get referred to palliative care very late in their disease trajectory, by which time the patient and the family have undergone most of the stressful journey on their own, without much hand holding in dealing with difficult situations. Early integration of palliative care, along with disease modifying treatment supports the patient and family by addressing all their issues, namely medical, social, financial, psychological and spiritual. As it functions with a multidisciplinary team, social workers, nurses, counsellors, volunteers, physiotherapists contribute to look after the patient in a holistic manner and provide support, comfort and care for the family.
Besides offering support, the team has important conversations regarding futility of aggressive therapy towards end of life with the patient and family and documents the wishes of the patient, so that the patient is given dignity and respect during his / her most vulnerable phase in life.
The number of people needing palliative care will increase due to the aging population and expected increase in morbidity and mortality from cancer
How does palliative care improve quality of life for a lung cancer patient?
Median survival for patients with locally advanced non-small cell lung cancer, defined as lung cancer involving regional lymph nodes, is estimated to be approximately 10 to 17 months, and median survival for patients with metastatic disease is only 6 to 9 months. In addition, patients with advanced lung cancer often experience debilitating symptoms and poor quality of life. Pain, shortness of breath, and fatigue are most frequently reported and affect at least 65% of patients with advanced lung cancer. Given this burden, of symptoms and high mortality, patients and their families facing a diagnosis of advanced lung cancer are in need of support. Palliative care, with its focus on addressing the emotional, physical, and spiritual sources of suffering utilizing the expertise of an interdisciplinary team, can provide this comprehensive support.
Palliative care is appropriate for patients at any point in a serious illness. Unlike hospice, palliative care is not limited by prognosis and may be provided at the same time as disease-directed therapies.
There is strong evidence underscoring the importance of integrating palliative care across the trajectory of lung cancer. The primary oncology team should routinely assess for pain and other symptoms, and regularly inquire about a patient's understanding of his disease and his goals of care. Specialty palliative care can provide an extra layer of support for patients with lung cancer and their families by helping with more challenging symptom management, psychosocial support, complex decision-making, advance care planning, and transitions in care.
Patients with lung cancer who are breathless, have chronic cough, severe pain, exhaustion, fear and depression and significantly reduced physical and intellectual activities qualify for inpatient or home palliative care. Knowledge about various methods used in palliative treatment allows one to alleviate symptoms that occur in an advanced stage of disease with an expected short survival period. Methods of oncological treatment that are often used in patients with advanced lung cancer include radiotherapy and chemotherapy. Drawing attention to the earlier implementation of palliative care is an objective of research carried out during recent years. Advances in surgical and conservative treatment of these patients have contributed to better outcomes and longer survival time.
Lung cancer often makes it hard to breathe. How does palliative care help ease breathing?
Patients with lung cancer can experience breathlessness due to multiple reasons:
- Smoking related underlying lung disease like, Chronic obstructive lung disease: COPD
- Tumour obstructing a large airway
- Pleural effusion, i.e. fluid collected in the lining of the lung when cancer advances
- Surgical removal of a part of the lung as treatment
- Side-effects of chemotherapeutic agents, can cause lung fibrosis
- Following Radiotherapy to the lungs
- Anemia due to poor nutrition, drugs etc
- General debility, loss of muscle mass and tone
- Anxiety
Download the E-Book below on Managing COPD. You will need to register for free.
Many of these conditions may not be reversible. A detailed assessment by the palliative care team helps identify the cause of breathlessness. Palliative care offers non-pharmacological and pharmacological measures to cope with the symptom. Counsellors can address anxiety and panic attacks that worsen breathlessness. Physiotherapists focus on breathing techniques. Families are also counselled about what they can do to offer comfort, for eg. Well-ventilated room, loose clothes, oxygen and nebulisers in select cases.
Pharmacological management in patients with optimum management of the condition is low dose morphine, given with close monitoring. It is an under-utilised wonder drug that has the potential to make the patient comfortable and offer suffering free days.
The treatment for lung cancer can be quite intensive. How does palliative care reduce toxic side effects?
Lung cancer is divided into two categories according to its biological characteristics and different ways of treatment. Non-small cell lung cancer (NSCLC) represents 80–85% of cases, while small cell lung cancer (SCLC) represents 15–20% only. Risk factors for lung cancer include smoking, passive smoking, exposure to asbestos (mesothelioma), ionizing radiation and certain metals. Lung cancer does not give a good prognosis. This is most commonly due to too late diagnosis, advanced age, coexisting diseases, and hence limited therapy.
The type of palliative care depends on the needs and may change throughout the lung cancer treatment process. Here are some examples of types of supportive care for lung cancer:
- Procedures to open airways
- Medications to treat pain like opioids
- Medications to suppress a cough, open closed airways and improve breathing like steroids
- Extra oxygen from small, portable tanks
- Medications to make you hungry
- Emotional support and counseling to deal with emotions and fear
- Nutritional supplements to reduce weight loss
- Medications to reduce nausea
- Drugs to treat bloody coughs
Is lung cancer palliative care appropriate at all stages of the illness, or just during end-of-life care?
Lung cancer palliative care is appropriate at all stages of the illness, not just during end-of-life care. It is perfectly okay for the patient to ask for supportive care for lung cancer. Palliative care provides relief from a variety of physical and emotional symptoms. Tracking symptoms can help the patient talk to their doctor who then can help get lung cancer supportive care.
With the increasing number of rise in cancer patients (1 lakh new cases of all cancers every year in India) it is not humanly possible for oncologists to spend time to explain and understand every patients’ requirements. Palliative care fills in just that gap in total care of the patient. Integrating palliative care with curative treatment is the ideal way for optimal use of expertise.
In recent years, numerous studies have been conducted with an objective to draw attention towards the implementation of early initiation of care provided by the palliative care team and specialist nursing care in patients with cancer. Published data show that the impact of the introduction of palliative care in patients with NSCLC (Non Small Cell Lung Cancer) at the time of diagnosis on changes in QL after twelve weeks of treatment. Participants were offered continuance of the standard oncology care only or the introduction of palliative care with standard oncology care jointly. Quality of life in the group where palliative care was introduced was higher in comparison to the group of patients who underwent only standard cancer care. Patients in the group in which palliative care was introduced in older age required less aggressive treatment. Another paper published, argued that palliative care should be implemented together with the standard oncology care immediately after diagnosis in patients with NSCLC. Early implementation of palliative care improves the QL and alleviates coexisting symptoms. The introduction of palliative care causes appropriate referral of patients to the hospice and reduces the use of futile intensive care.
Unfortunately, currently this is not the scenario in India. In many patients, palliative care team is involved only when the oncologists have no further curative therapy to offer. Patients get referred to palliative care, “when nothing more can be done”! This statement completely squashes hope and the will to live of the patient. With the help of palliative care comfort of the patient becomes a top priority and care of the family members crucial.
Who provides palliative care? Are there trained palliative care specialists?
Doctors who are specially trained in palliative care will manage your treatment. They work with the oncologist or primary-care doctor to update on the patients’ progress.
Palliative care team includes
- Nurses or nurse practitioners
- Home health aides
- Social workers
- Psychologists
- Breathing therapists
- Pharmacists
- Dietitians
- Clergy
- Volunteers
Does palliative care impact overall survival or prolong life in lung cancer patients? Does it increase the will to live?
As mentioned earlier, research has been done in a specific type of lung cancer, NSCLC and proved that palliative care introduced early has a significant positive impact on patient quality of life. Patients receiving palliative care were reported to live longer.
In any chronic progressive, disease receiving constant supportive guidance, counselling and effective symptom control will surely make any patients’ difficult journey bearable. This is the fundamental objective of palliative care.
Do you think palliative care should be integrated with standard oncologic care from the beginning of treatment?
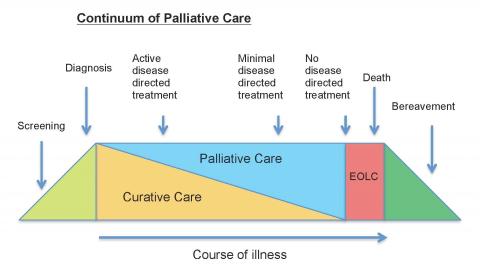
Definitely. There is a lot of research done regarding benefits of early integration of palliative care even in oncology. Palliative care helps patients adhere to curative treatment, hand holds them through side-effects, counsels them during difficult times and by avoiding unnecessary medical intervention improves overall quality of life in patients with cancer. Unfortunately, most patients receive palliative care towards the end only, making their disease experience traumatic. The following diagram shows the ideal time to introduce palliative care is as early as possible.
Is palliative care only for patients or does it also extends to family members and caregivers?
As per the WHO definition, palliative care aims to improve quality of life of patients and their families in a holistic manner. We fail to recognise the burden, stress, frustration of carers when they look after chronically or seriously ill patients. It takes a toll on the family in every way, socially, psychologically, financially and spiritually. It is important to look after the patient and his family so that both are in a state of mind to receive help, support and guidance.
As a palliative care physician, how do you think the palliative care movement in India can be given impetus?
Currently, we are at the point where we need to focus on spreading awareness and push the diffusion of innovation curve. Hard work done by Dr. M.R. Rajagopal and many senior doctors since 20 plus years has resulted in many positive changes. The Supreme Court of India has accepted the right to refuse treatment by the patient as legal. Further, the amendment of the Narcotics and Psychotropic Substances Act, NDPS 2014, and the recent judgment by the Supreme Court regarding upholding of advance directives and “Living will”, especially in conditions with no cure available.
We need to focus on increasing awareness in the community, educate doctors in government and private hospitals, train medical students from under graduate level in the concepts of palliative care, medical ethics and communication skills. There has to be a paradigm shift in the thinking process of the physicians and patients to see a change. Presently, according to a published report in the Lancet, 2015, India ranks amongst the 15 worst countries to die in. There is so much work to be done to improve this statistic, as death is inevitable bad death is avoidable.
(Dr Rajam Iyer is a pulmonologist and palliative care physician with Bhatia and Hinduja Hospitals.)