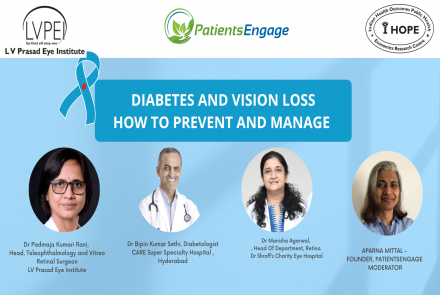
Diabetic Macular Edema or DME is a growing concern in India especially because it is most prevalent in persons with Diabetes. Learn more about the causes, symptoms and treatment options available for DME. Dr. Padmaja Kumari Rani, Network Head, Tele-ophthalmology and vitreoretinal surgeon at L V Prasad Eye Institute provides valuable information on treatment and prevention of DME.
What is Diabetic Macular Edema?
Diabetic Macular Edema (DME) is a condition that affects the retina, particularly the macula, which is responsible for central vision. In individuals with diabetes, high levels of blood sugar can lead to the accumulation of fluids and proteins in the retina, causing the normally transparent membrane to become thickened and distorted. This results in blurred or distorted vision, like a camera's lens becoming foggy or obstructed. DME is detected through dilated eye examinations, where drops are used to widen the pupil, allowing for a clearer view of the retina. In affected individuals, the macula may show yellow or red spots indicative of fluid buildup and thickening, impairing central vision and potentially leading to vision loss if left untreated.
What are the symptoms of DME?
Diabetic Macular Edema (DME) is a vision-threatening complication of diabetes that affects the central part of the retina, leading to potential vision loss. Typically, DME presents with symptoms such as blurred vision. Patients may initially attribute this blurriness as a need for new glasses, especially if they are in the age group of 40 to 50 years old, but correction with glasses will not resolve the issue. The blurred vision persists due to fluid buildup and thickening in the macula, impairing central vision. It's important to note that in Diabetic Retinopathy, which is the condition leads to DME, there may be no noticeable symptoms until it progresses to DME. Hence, regular eye examination is crucial for early detection and treatment.
Is DME a complication of Diabetic retinopathy?
Yes, Diabetic Macular Edema (DME) is a type of diabetic retinopathy. In diabetic retinopathy, the retina, which is normally a transparent membrane, can be affected by the accumulation of glucose, leading to changes in its structure and function. Initially, in mild cases of diabetic retinopathy, patients may only exhibit small red dots within the retina. However, as the condition progresses, diabetic macular edema occurs, characterized by the accumulation of fluids and proteins in the central part of the retina, known as the macula. This thickening of the macula leads to the appearance of yellow and red dots and results in visual disturbances, particularly blurred vision. While not all patients with diabetic retinopathy will develop diabetic macular edema, it is a common complication, occurring in approximately 10% of those with diabetic retinopathy.
What are the various risk factors for Diabetic Macular Edema?
The primary risk factor for diabetic macular edema (DME) is diabetes itself. However, several other factors can contribute to its development. DME is more commonly observed in individuals with type 2 diabetes, particularly in older individuals who may also have obesity. Additionally, abnormalities in lipid metabolism, known as dyslipidemia, and hypertension are significant risk factors for DME. Patients with diabetic nephropathy, a kidney complication of diabetes, are also at a risk of developing DME. Individuals with diabetes who have concurrent cardiovascular conditions may face an increased risk of retinopathy and macular edema.
Overall, DME is often associated with the presence of multiple complications of diabetes, reflecting the importance of comprehensive management of the disease and its associated conditions.
Types of DME
Diabetic macular edema (DME) can be classified into three types based on the severity of the condition.
- Mild DME: In this type, yellow or red dots are observed in the retina, but they are located away from the central area known as the fovea. Patients with mild DME may not experience significant visual impairment.
- Moderate DME: Yellow and red dots become more prominent and begin to approach the central area of the macula. At this stage, patients may start to experience mild to moderate visual disturbances.
- Severe DME: This type is characterized by a significant accumulation of yellow spots, or hard exudates, in the central part of the macula. The entire center may be affected, leading to severe vision loss for the patient.
By categorizing DME based on its severity, healthcare professionals can better understand the extent of the condition and make treatment plans accordingly to manage and minimize vision loss.
Treatment of Diabetic Macular Edema
There are various treatment options available for Diabetic Macular Edema. The primary cornerstone of treatment is maintaining good control of diabetes and managing associated systemic conditions such as hypertension and dyslipidemia. For mild DME, systemic control through measures like maintaining HbA1c levels around 7, controlling blood pressure below 130/85, limiting salt intake, adopting a healthy lifestyle with regular exercise and dietary changes can be effective.
For moderate to severe DME, intravitreal injections are often recommended. These injections target vascular endothelial growth factor (VEGF), a factor responsible for causing leakage from blood vessels and swelling in the macula. These injections, known as anti-VEGF injections, aim to inhibit VEGF activity and reduce macular edema. Additionally, steroids may be administered as injections into the eye if anti-VEGF treatment is not effective. Steroids help reduce inflammation associated with DME.
In summary, the treatment approach for diabetic macular edema typically involves a combination of systemic control and intraocular injections, tailored to the severity of the condition and the individual patient's response to treatment.
Can DME be prevented? How the progression of DME can be slowed?
Preventing diabetic macular edema (DME) and slowing its progression involves addressing both systemic factors and direct treatment of the condition. While DME itself may not always be entirely preventable, managing diabetes and associated systemic conditions significantly reduces the risk of its development. Controlling blood sugar levels, maintaining blood pressure within a healthy range, and managing dyslipidemia are crucial steps in preventing DME. Furthermore, the progression of DME can be slowed with appropriate treatment. Injections targeting factors like vascular endothelial growth factor (VEGF) and inflammation can reduce macular swelling and improve vision.
However, it's essential to understand that these injections act as a form of physiotherapy, providing symptomatic relief. The underlying cause of DME is diabetes, so controlling diabetes is the main thing for long-term management. For individuals with concurrent kidney disease or other systemic complications of diabetes, comprehensive management of these conditions is essential alongside DME treatment.
By addressing both systemic factors and directly treating DME, the progression of the condition can be effectively prevented, leading to better outcomes for patients.
How often should someone get screened for DME? And is it done during the same screening for diabetic retinopathy for diabetic patients?
Screening for diabetic macular edema (DME) should be conducted regularly, especially for individuals with diabetes. The frequency of screening depends on the type of diabetes and individual risk factors. For individuals with type 1 diabetes, screening for DME should begin within five years of diagnosis and continue regularly thereafter. In contrast, for those with type 2 diabetes, screening should commence immediately upon diagnosis due to the potential for delayed detection of diabetes.
Screening for DME is typically integrated into diabetic retinopathy screening. Therefore, during a comprehensive eye examination for diabetic retinopathy, healthcare providers also assess for the presence of DME. This examination involves dilating the pupils to allow for a thorough evaluation of the retina and macula. For individuals above 40 years of age, or those with a family history of diabetes, hypertension, or dyslipidemia, regular eye check-ups are recommended as part of preventive healthcare.
Early and regular screening for DME is crucial as it allows for timely detection and intervention, potentially preventing vision-threatening complications. Additionally, effective management of diabetes, especially in the early years after diagnosis, can significantly reduce the risk of developing diabetic retinopathy and DME through the concept of metabolic memory or the "legacy effect." Therefore, maintaining good control of diabetes from the outset is essential for long-term eye health and reducing the risk of complications such as DME.
Is there any association between pregnancy and diabetic macular edema (DME)?
Pregnancy can impact the risk of developing DME due to hormonal changes and physiological alterations in the body. Women who experience gestational diabetes during pregnancy have an increased likelihood of developing DME.
Additionally, pregnant women with pre-existing diabetes are also at a higher risk of DME due to possibilities of diabetic retinopathy and pregnancy-induced changes in amniotic fluid retention. Regular eye examinations during pregnancy, particularly in the first trimester and throughout gestation, are essential for early detection and management of DME to prevent vision-threatening complications. Postpartum follow-up is essential to assess the long-term risk of developing diabetes later in life and to monitor for diabetic retinopathy and DME.
“Diabetic Macular Edema (DME) is characterized by changes in the retina's transparency and the accumulation of yellow and red dots, leading to thickening in the central part of the macula. This condition affects vision and can range from mild to severe, impacting individuals with diabetes. Regular eye examinations are crucial for early detection and management of DME to prevent vision loss.”- Dr.Padmaja Kumari Rani

Dr. Padmaja Kumari Rani (Network Head, Tele-ophthalmology and vitreoretinal surgeon at L V Prasad Eye Institute, Adjunct Associate Professor of ophthalmology at The University of Rochester, New York)