Thousands of Indian women undergo hysterectomy, or removal of the uterus, every year, even though most of these cases can be avoided. Dr Shital Raval enumerates some surgical and non-surgical options available that should be considered before opting for hysterectomy.
Hysterectomy is a surgery that entails partial or complete removal of the uterus in women. In America alone, more than half a million women have a hysterectomy every year. Is it a necessary surgical option? Or are there alternatives that you can condider for various medical conditions?
Some claim that 90% of the hysterectomies are unnecessary and can be avoided. In certain cases, especially cancer, elective hysterectomy is recommended and essential. Hysterectomy can be total (removal of entire uterus and cervix) or partial (ovaries and cervix are left whole). If the ovaries and fallopian tubes are also removed, it is referred to as Bilateral salpingo-oopherectomy or BSO.
When is hysterectomy necessary?
- In women with cervical cancer, uterine cancer or ovarian cancer
- Excessive or sudden uterine hemorrhage
- Severe uterine infection
When is hysterectomy necessary only as a final option?
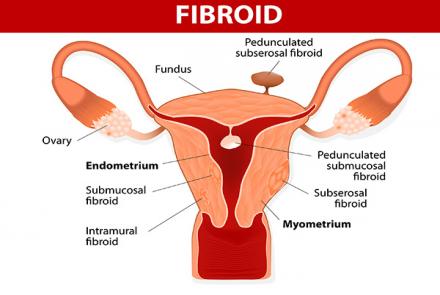
- Uterine fibroids
- Endometriosis
- Uterine prolapse
- Abnormal vaginal bleeding
- Adenomysosis (abnormal endometrium growth)
- Uterine polyps
In many of these cases, hysterectomy can be avoided and other alternatives should be offered to the patient. Non-surgical options are available and should be considered before opting for hysterectomy. This also helps preserve fertility and prevents complications related to a hysterectomy like early menopause, difficulty in urinating and weakened pelvic muscles.
Be sure to check with your doctor and get a second opinion as a hysterectomy is a permanent procedure. With advancement of medical research, there are increasing number of options now. So spend time to evaluate the options before making any final decisions.
Alternative treatment options for various conditions:
| CONDITION | TREATMENT CHOICES |
|---|---|
|
|
|
|
|
Uterine Prolapse |
|
|
Vaginal bleeding |
|
|
Adenomysosis |
|
|
Polyps |
|
So take the time to understand the options available to you and seek a second opinion if need be.
#BeAware #BeEmpowered