Living with COPD is tough but with interventions like pulmonary rehabilitation, physical activity, self-management, and nutrition, it is possible to improve social and mental well-being. Understand the causes, complications, management options with our panelists: Dr. Pralhad P. Prabhudesai, Chest Physician and Bronchoscopist Poorvi Devani, Respiratory Physiotherapist
Note below the time stamps of the video recording
(3:19)What is COPD? What are the main types?
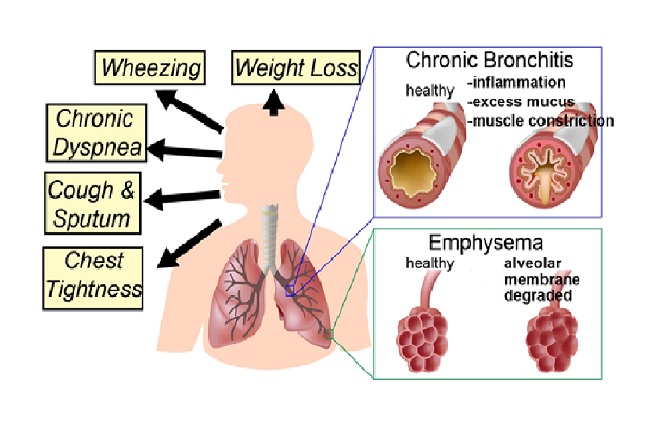
As the name itself suggests, it is chronic, it is obstructive, and it is a lung disease. Obstructive means the airway becomes narrow due to friction that causes swelling or inflammation in that area. The other reason is the thickening of the alveoli, which are the grape-like structures attached to the bronchioles (terminal part of the airways). Usually, the alveoli are very elastic and potent keeping the airways passages open. In emphysema, the alveoli become thick, making the air passage narrow. Majority of the COPD patients have destruction of their alveolar walls which causes the narrowing of airways. The function of the alveoli is to transfer oxygen and carbon dioxide between the air and the blood capillaries. If the alveoli are destroyed, the capillaries also lose their gas exchange units leading to lack of gas exchange.
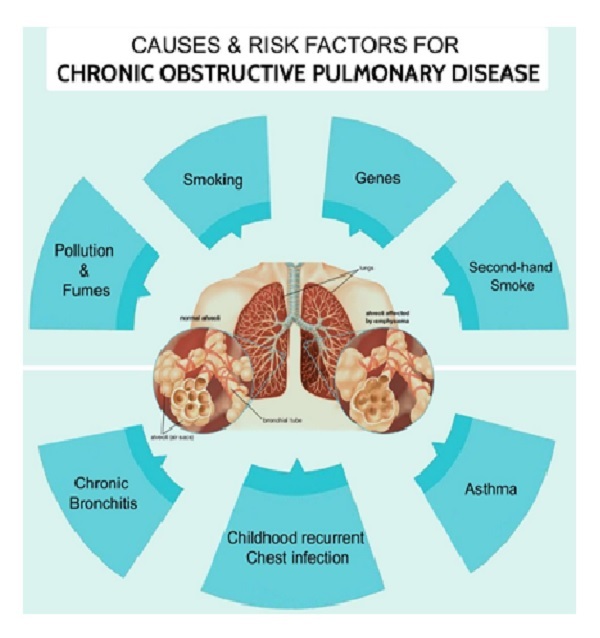
COPD is generally categorised into Chronic Bronchitis and Emphysema. Most common cause is smoking but there is also non-smoker’s COPD. This is seen in persons exposed to biogases such as females using wood for cooking. Other reason is exposure to air pollution. Indoor pollution due to incense burning, mosquito repellent or coil use which lead to constant irritation of the airways similar in pathology to what the smokers get. The last cause is genetic. Certain genes are responsible for promoting cellular destruction while others promote lung health which creates a good balance. When there is an imbalance, there is worsening of the lung health and more so in person with risk such as smokers etc. This is the crux of COPD.
Important complaints of COPD are chronic cough, sputum, wheezing, chest tightness and weight loss in some due to the constant breathlessness.
(8:15) Is Asthma a COPD?
Asthma falls under allergic conditions where the inflammation of the bronchi and bronchioles is allergic in nature and onset. This is called Eosinophilic disease because it causes increase in the number of eosinophils. Eosinophils are generally high when there is an allergic reaction. The diagnosis and concept of treatment is very different compared to COPD. Hence it is not the same or a COPD.
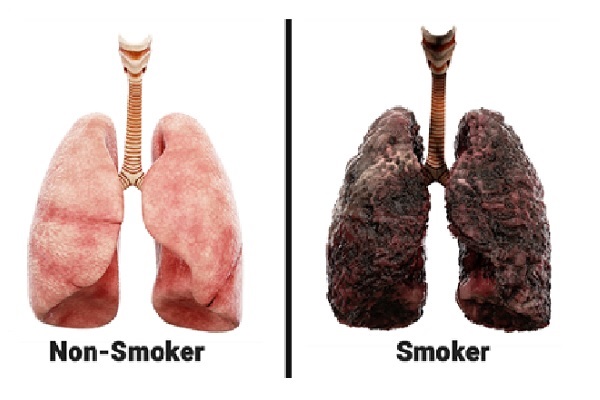
(9:16)Difference between a smoker and a non-smoker’s lungs?
A healthy lung is as the picture shows whitish in colour, a child’s lungs are pinker. While a smoker’s lungs are black and even his sputum may be black. This is because of the accumulation of carbon particles in the lung tissue.
(10:09)Causes and Risk factors of COPD?
These include smoking, pollution & fumes, second-hand smoke, history of Asthma or Chronic Bronchitis, frequent chest infections during childhood and alpha 1 antitrypsin deficiency. Asthma is a risk factor because some who get afflicted with asthma and don’t mange it well, have symptoms that behave like COPD. Few people claim that untreated asthma leads to COPD but remember in COPD, there is an emphysema aspect that is never seen in Asthma. However, there is often a doubt, when you first see a patient because it is not easy to differentiate on observation alone.
Alpha 1 antitrypsin is an enzyme formed in the liver. There are two important enzymes: trypsin and anti-trypsin. Trypsin causes alveolar wall destruction while anti-trypsin prevents the action of trypsin. If there is a deficiency in anti-trypsin, the balance will tilt towards the trypsin action. A person with such a deficiency will show COPD early in their life esp. signs of emphysema. So, a young person who presents with emphysema may be a likely candidate of Alpha 1 antitrypsin deficiency, while an older person may be a COPD patient. If the deficiency is diagnosed, external Alpha 1 antitrypsin can be given but this is an expensive therapy. There can also be partial deficiency which can present later in life. This can cause complications in smokers and person with other risk factors. A characteristic sign of Alpha 1 antitrypsin deficiency is that it is seen in the lower lobes while COPD is seen in the upper lobes.
(13:49)Is it difficult to diagnose COPD?
It is not difficult, but it is often missed. It is not diagnosed clinically by a stethoscope but needs spirometry or a lung function test for diagnosis. On spirometry, if the FEV1*/FVC ratio is less than 70, then it is an obstructive lung disease. Then this is compared to normal FVC and categorised into mild, moderate or severe disease. A complete lung function test includes lung volume measurement, diffusion test and spirometry. It is simple and cheaper than a Chest X-ray.
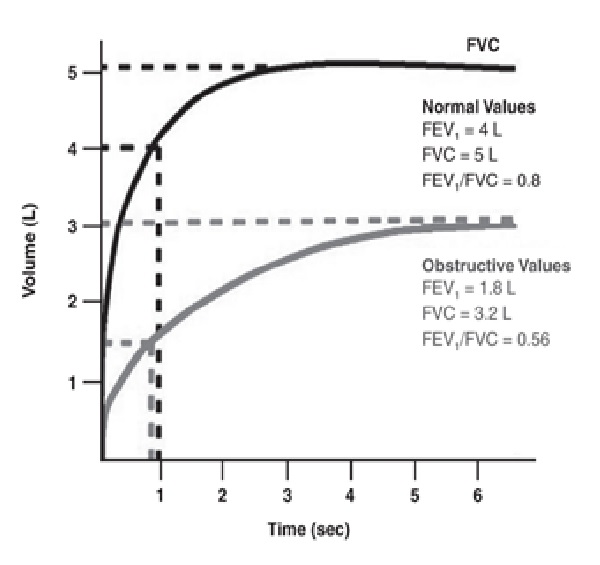
FEV=Forced Expiratory volume
(16:08) What is the ABCD Assessment Tool?
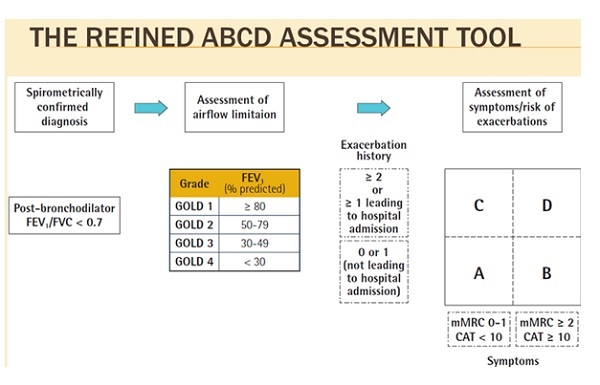
The ABCD assessment is a tool (used since the last 3 years) to assess the patient’s disease status. There is a CAT score and mMRC score (for breathlessness) in a grid which notes the exacerbations and number of hospital admission. A patient is graded A,B,C or D based on these two parameters. If you are A, you have less exacerbations and hospital admissions compared to D who highly has both. This grid helps the doctor determine the course of treatment. One should never look at just the FEV1 values. Even if the FEV1 values are very low, the patient may fall in the A group with less symptoms and no exacerbations. Contrastly, a patient may have good FEV1 values but may being the C or D group depending on their exacerbations. Hence the GOLD Guidelines help decide how to manage patients. Further treatment will depend on how severe are the symptoms and how many exacerbations the patients has had.
(19:40)What are the common treatment goals?
All COPD patients should firstly avoid exposure to pollution (both outdoor and indoor) and smoke. Smoking cessation is vital for all cigarette/bidi smokers. Next vaccination is a must; generally, this includes the annual Flu vaccine and the Pneumococcal vaccine every 5 years. Health education is important for all these patients along with Pulmonary rehabilitation for the symptomatic patients. There are many aspects to this which a Respiratory therapist can assist with. As per as medical treatment is concerned, it depends on which group the patient falls into.
| A group | Bronchodilator alone (like salbutamol or ipratropium) |
|
B group C group |
Combination of long acting β2 agonist + Anticholinergic |
| D group | Combination of long acting β2 agonist + Anticholinergic +Inhaled Steroid and/or Theophylline like drugs plus Macrolides and Antibiotics to prevent hospitalizations. |
Patients from B and D group must get on the Pulmonary Rehab Program as well.
Bronchodilators are used in milder patients.
(23:08)What are the benefits of Pulmonary Rehabilitation?
- Patient education about their disease.
- Learning about their medications and how to take them.
- Improving functional capacity to reduce their dyspnoea (breathlessness) by doing the prescribed exercises.
- Help in dealing with the psychological aspect of the chronic disease especially emotional health.
- Number of hospitalizations and visits to Doctor’s clinics are reduced as patient learns to manage minor exacerbations on their own.
- Improvement in quality of life.
(25:05)When should a patient start rehabilitative care?
According to the GOLD guidelines, rehab should be offered to all patients, especially those who are symptomatic. Rehab can be started in the hospital when the patient is admitted. Even in the ICU, physiotherapy can commence and then continued in a clinic when the patient is in the subacute phase. Patients who are immobile and fragile can get Rehab in their own homes.
Before rehab starts, every patient must get a clean chit from their Chest Physician that they are fit for rehab. Secondly the patient must be compliant with all their medications. Each patient will be given a customised exercise plan after initial assessment of their lung strength and capacity. Both aerobic and strength training is done using dumbbells, thera-bands, stationary bikes etc. It is a gradual progress and after 6-8 weeks, another assessment is done to evaluate progress. Adherence to the program is very important for any progress to occur. In order to make sure the patient is motivated and stay motivated, we refer to their initial assessment to check for their goals. For example, some patients complain to being unable to go to their temple or climb the stairs, so we use that goal to motivate them. Once such small goals are achieved, we use these objective measures to show them improvement in their condition. This also helps them gain faith and confidence in their Physiotherapist which in addition helps them do better.
(31:50)Is there a relationship between COPD and Lung Fibrosis?
COPD is an obstructive disease while Lung Fibrosis is a restrictive disease. Lung is like a sponge; when you compress it air comes out. If you put fevicol on one part of this sponge, then that part become crumbly and loses it sponginess. Similarly, if there is scarring or fibrosis, less amount of air is able to go in and out of that area. There are many types of fibrosis. For instance, in Interstitial Lung Diseases, the scarring is in the interstitium of the lung (the area between the alveolar wall and the capillary wall where exchange of gases takes place). When this interstitium gets thickened, it is called fibrosis. This can extend into the pleural space too, leading to loss of lung volume and restriction.
In COPD, the lungs become hyper-inflated and large, giving the characteristic barrel-shaped chest.
(35:42) Please explain the difference between an inhaler and nebuliser?
Nebuliser and Inhaler are both aerosol generating devices. Inhaler can be meter-dosed which when pressed provides a fixed dose of medicine in each flow. The medicine flows from the canister and comes out with a propellant. Inhalers can have one or a combination of up to 3 medicines in it. It can also have a dry powder in the same way, but one has to inhale it deeply so that the powder reaches the lungs. So, the inhaler can be in a dry powder form or a metered dose.
Nebuliser is a machine that forms a cloud or nebula of the medicine, so you get a large amount of dose going into the system. The medicine along with saline is provided (can be pre-mixed) to put into the tube. This is attached to the nebuliser chamber where it becomes a cloud and can be inhaled by the face mask. This mask can be won over the nose or the nose and mouth and just breathe regularly, no inhalation is required like in the inhalers. This may take longer but a larger dose of medicine goes in as well compared to the inhaler. Nebulisers are usually given to patients who are in acute attack phase and so breathless that they cannot use the inhaler. A lot of medicine does get wasted but it is the easiest way to get large doses into the patient. It is regularly prescribed for patients with COPD and Asthma and can also be used to deliver antibiotics.
(40:15) When are patients put on portable oxygen? Difference between Oxygen cylinder and concentrator?
Oxygen (O2) cylinders come in varying sizes based on capacity. The large cylinders are heavy and not easy to move around, they also have a valve which may be tough to turn. Depending on your prescription (e.g., 1,2,3 litres of oxygen per min), you will need sufficient O2 handy for use in a day. O2 cylinders are ideal for short-term usage or for the terminally ill patients.
The oxygen concentrator is a completely different concept whereby the machine takes the atmospheric air, removes the nitrogen and delivers just the oxygen to the patient. Some mount of O2 does get recirculated back into the room, so that the room does not become oxygen deprived. This machine work son electricity and can go on for 24 hours with maybe an hour’s rest in between. It can be as large as 5 litres in capacity. Concentrators are recommended for patients who require long-term O2 therapy at home.
Concentrators are of two types: Continuous and Pulsated. When we breathe in, we need the oxygen but when we breathe out, oxygen is not required. The machine understands this and provides oxygen only when you inhale. When you exhale, the machine shuts off giving the battery a rest as well, thus making it longer lasting. This pulsated flow is suitable for a COPD patient. If the patient is breathing heavily, such as an ILD patient, then continuous flow is required.
Nowadays portable O2 concentrators are available for travel which are battery-driven. This has made travel much easier and can last on air trips till US and UK. Additional batteries should be carried for long hauls. If patients are travelling by car, the battery can be charged in the car itself. This has truly changed the management of COPD and ILD patients and made them more mobile.
(46:31) Does pollution in the winter cause flare-ups and how can patients avoid them?
Pollution is season dependent. Post monsoon, there is least pollution because there is less particulate matter in the air. In winter, as the temperature drops, pollution increases with the accumulated fog. This is responsible for triggering asthma and COPD. Other causes of pollution include Diwali and celebratory fireworks, sandstorms, and forest fire fumes that migrate to the nearby cities. There are many un-preventable factors but the ones a patient can prevent, he should avoid such as taking walks early foggy mornings or in crowded or trafficked areas. Wearing a mask is a great way to filter some of the air that is inhaled. During the lockdown, we a significant decrease in flare-ups because of no traffic and clean air. Indoor pollution is equally important so avoid incense/dhoop fumes, cooking smoke, insect repellents etc.
(49:49) What is the psychological help that patients need to get back to normalcy after an acute attack?
Most patients tend to lose their confidence post an acute attack. Frequent hospitalization due to disease chronicity causes disruption of daily routine along with the aftermath of weakness and fatigue. Anxiety of recurring acute attacks is also very real for some patients. A lot of time is spent on patient education at the clinic and during rehabilitation sessions. Due to immobility, COPD patients have a higher likelihood of systemic manifestation of depression and anxiety. With rehabilitation, 90% of the patients’ psychosocial problems are solved. However, some patients may require additional counselling as there may be an underlying element of mental health issues which are independent of COPD. In such cases, psychiatric care is required.
(53:15) During the lockdown, did methods of rehabilitation change?
Due to the COVID pandemic, our centres were shut down, but we were able to shift to tele rehab sessions. It was a smooth transition since we had carried out a few trials before the lockdown started. We are now doing online session for the past 8 months. For the elderly, we have found that WhatsApp video calls are the simplest method.
(55:13) Patient question: I have to exert to breathe at night. Do I need to start any meds, am currently not taking anything for my COPD?
Patients of all chronic lung diseases tend to have worrisome nights; this may be due to several reasons. One of the reasons could be diurnal variation that happens in the airways just like how BP changes at night-time. This may cause worsening of breathlessness. Second reason may be due to heavy meals at night-time. This causes the abdomen to get distended and consequently puts pressure on the diaphragm and the chest cavity where the lungs are housed. When a person is horizontal, the entire lung compartment’s position changes along with circulation and this in turn affects the gas exchange. Hence, lying down start after dinner causes discomfort and shortness of breath. Third reason is that patients are preoccupied during the day but at night when they are more free, they dwell on their disease. Taking all of this into consideration, a patient should be assessed and advised changes to lifestyle, food habits, diet, breathing techniques and avoiding overthinking.
(58:40) Patient question: Why do I produce a lot of saliva at night even though I’m using the Oxygen concentrator?
Saliva production is normal, and we usually swallow it down. Certain medicines cause increase in saliva production while others (like certain anti-cholinergics) cause complete dryness in the mouth. If the patient has any oesophageal issues, then saliva does not go down into the stomach and instead collects in the mouth. This are minor issues and can be easily managed. Dryness of the mouth is more of a concern for patients especially those who are mouth breathers. If dryness is due to an underlying autoimmune disorder like Sjogren’s or Sarcoidosis, then steroids can improve dryness.
(1:01:38) Steroids have many side-effects, which ones do you regularly encounter and how are they monitored?
Steroid is a double-edged sword! It has many benefits but comes at a cost. There are numerous side-effects:
- Gastritis and hyperacidity which can form stomach ulcers and worsen existing ones.
- Fragile bones because it drains calcium out of the bones. This can lead to increased fractures esp. in the spine and hips.
- Steroids are innately produced in the body by the adrenal glands when signalled by the Pituitary glands. There is an existing biofeedback mechanism for production of adrenaline/steroid in the body. If a body is provided with external steroid constantly, then this biofeedback mechanism is lost. Hence when external steroid is withdrawn, the body goes into steroid deficiency. This causes tiredness, fatigue, metabolic imbalance etc.
- Metabolic changes such as water retention, bloating, weight gain, moon-like face, unwanted hair on the face are commonly seen.
- More serious side-effects which need to be monitored regularly include glaucoma, early cataracts, increase in BP, Diabetes, bruises on skin, papery skin etc.
(1:06:08) Patient question: Is an air-purifier useful and effective?
Air purifiers are useful but not everyone should buy one. It should be based on a person’s needs and environment. Severe asthmatics may benefit as the air purifier makes the air drier by removing the water density, plus it decreases the dust mites in the air. Some new purifiers claim to filter out bacteria, viruses and fungi/mold from the room too. If you house is in a heavy trafficked area, then it may be beneficial to have a purifier in the house.
(1:07:36) Patient question: What is the best time to go for a walk?
Pollution should not be taken as an excuse to avoid walking. In cities like Mumbai, where pollution is thick especially in winter, one should avoid the early morning walk when the fog is low. However, patients can walk a little later in the morning when the fog has lifted, and this is a great way to start the day. Don’t leave it till the evening as you may get tired and busy by the end of the day.
(1:08:32) What is assisted cough?
This is a technique taught to patients to help remove phlegm stuck in their airways. There is more cough production in the morning time after a patient has been lying down for 6-8 hours. Patients are given tactile stimulation with hands and prompted to take a deep breadth and then cough to forcefully remove excess phlegm.
(1:10:20) What is COPD bloating?
Bloating in general causes a lot of discomfort and significantly increases breathlessness for a COPD patient. If there is constipation or gas formation, there is distention of the colon and pressure on the surrounding organs. This pressure is also felt in the chest leading to discomfort. COPD patients are more affected because they have a tight diaphragm with restricted movement compared to a normal person. Such patients should be advised a special diet by a dietician to increase their fiber intake and adopt ‘smart-eating’ diet which is consuming good proteins and calories but in less quantities. All COPD patients are provided a consult with a nutritionist so that they maintain a good BMI. This is because a large number of patients do lose weight while there are many who are overweight or obese. Patients with low BMIs are encouraged to improve body weight with good muscle mass. If such patients continue rehab without a good diet program, they may lose weight further. Hence nutrition is the second most important component of Pulmonary rehab.
(1:14:10) In post COVID patients, are there likely to be fibrosis or COPD symptoms? Are these permanent or curable?
COPD is not known to occur because of COVID. COVID patients may experience some fibrosis, hyperreactivity or cough but none of these are permanent. All lung infections are followed by scarring of the lungs and this healing may take some time, but patients do come out of it. In very few cases, the fibrosis was seen to last longer.
(1:15:30) Should COPD patients take the COVID vaccine?
The COVID vaccine will be taken by everybody including all the chronic lung disease patients. For live virus vaccines, more studies will be required to evaluate their reactions and effectiveness.