There is increased global awareness of Long-Covid. Dr Arvind Nune, Consultant Rheumatologist & General Physician in the United Kingdom explains Long-Covid symptoms, how to diagnose and manage Long-Covid.
What is Long-Covid?
Some patients recuperating from acute COVID-19 infection develop various symptoms that may last for several weeks to months. This has been widely known as “long Covid”.
Long-Covid is defined as a long-term sequel of a SARS-CoV-2 infection, presenting as continuous or relapsing and remitting symptoms several weeks after recovery from infection. The National Institute for Health and Care Excellence (NICE) defines the post-COVID-19 syndrome as symptoms that arise during or following an infection consistent with COVID-19. These symptoms persist for more than 12 weeks and cannot be attributable to an alternative diagnosis.
In October 2021, World Health Organisation (WHO) has defined long COVID as “post COVID-19 condition” which occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 infection with symptoms that last for at least 2 months, which cannot be explained by an alternative diagnosis.
What is the incidence of Long-Covid in India?
We do not know the true extent of long-Covid sufferers in India. Based on 2.1% of the UK’s population developing long-Covid, we can estimate that 27.6 million of Indian population may be affected by long-Covid.
An estimated incidence of long-Covid following COVID-19 infection has been reported to be up to 2.1% in the United Kingdom (UK). As cases of COVID-19 cases continue to increase, we will alongside see increase in cases of long Covid. In the long run, this will add to the burden that long-Covid will pose on the global healthcare systems.
What are the symptoms of Long-Covid?
Long-Covid symptoms can differ from person to person. The most commonly reported long-Covid symptoms include breathlessness, cough, fatigue, joint pains, sleep disturbance, brain fog and muscle pains. As per the UK Office of National Statistics, the most common self-reported long-Covid symptom was fatigue (58%) followed by breathlessness (42%), muscle aches (32%) and difficulty in concentration (31%).
Why is it difficult to diagnose Long-Covid in some patients?
It is usually straightforward to diagnose long-Covid. However, it might be slightly difficult to diagnose it in some patients as some medical conditions have symptoms that are similar to long-Covid. These include Systemic autoimmune rheumatic diseases (SARDs), including rheumatoid arthritis (RA), connective tissue disease (CTD), inflammatory myositis (IM) and fibromyalgia (FM) and chronic fatigue syndrome (CFS). Many of these conditions share similar clinical features such as joint pains, muscle pains, fatigue, and breathlessness. Similarly, respiratory ailments such as Asthma and chronic obstructive pulmonary disease (COPD) can also cause breathlessness.
Patients with a previous diagnosis of COVID-19 infection and a history of rheumatic diseases, who have developed persistent joint or muscle symptoms pose a substantial challenge to clinicians. Their symptoms could be due to long Covid or a flare-up of their pre-existing rheumatic disease. Therefore, patients should consult a local clinician to confirm the diagnosis if there is any doubt.
How is Long-Covid diagnosed?
Long-Covid is primarily a clinical diagnosis. The diagnosis of long-Covid can be made based on a patient’s symptoms with or without a positive SARS-CoV-2 test (PCR, antigen, or antibody). Long-Covid remains a diagnosis of exclusion, and patients should be appropriately evaluated before reaching a final diagnosis.
A careful history, physical examination and appropriate investigations will enable clinicians to arrive a final diagnosis if there is a diagnostic dilemma.
Why do some patients develop long Covid and others don’t?
Currently, it is unknown why some patients develop long-Covid while others do not. Although this is evolving, some studies have shown that severity of COVID-19 pneumonia, Intensive care admission, older age and female sex predict severity and persistence of long-Covid. It is logical that vaccination against SARS-CoV-2 does reduce the risk of long-Covid. Without having a COVID-19 infection, patients would not develop long-Covid. Vaccination against SARS-CoV-2 infection is thus the most effective way to prevent long-Covid.
What is the prognosis for those with long COVID?
We don't have a clear picture of the prognosis yet. According to studies, long Covid symptoms can last anywhere from a few weeks to months. In our study of 89 acute COVID-19 survivors from the United Kingdom, we found that nearly half of them still had long-Covid symptoms 9 months later. More than a third of our patient cohort had multiple long-Covid symptoms. However, the good news is that patients can alleviate their long Covid symptoms with holistic measures.
How can patients work on improvement of symptoms?
Although a multi-disciplinary approach is the mainstay of treatment for long Covid, patients can improve their long Covid symptoms in a variety of ways.
- Learning how to pace oneself can improve fatigue.
- Mindfulness activities such as Tai Chi, yoga and swimming can help improve long-Covid symptoms like fatigue, sleep pattern and other cognitive functions.
- Coping and managing pain with appropriate pain relief is also an important part of managing the symptoms.
- Relaxation and breathing exercises may help alleviate breathlessness.
Patients should consult their clinicians if symptoms persist despite the initial measures.
Are there any treatments available?
There is no cure or any specific treatments available for long-Covid. Once we understand what might be causing the disease, we may find treatments. The current strategy is to prevent long-Covid by preventing COVID-19 infection. This also emphasizes the importance of employing barrier methods against SARS-CoV-2 infection such as face masks and sanitization.
How does long-Covid be managed?
Because of the complexity of the clinical syndrome, long Covid management should ideally involve a multidisciplinary approach. Long-Covid clinics in the United Kingdom include occupational therapists, physiotherapists, and clinical psychologists to provide a holistic approach to management. We understand that long-Covid MDT clinics are unavailable in many low and middle-income countries (LMIC) due to a lack of resources. Given the varying quality of health-care delivery, we recommend that patients adhere to country-specific guidelines.
Raising awareness and education about the condition among clinicians and patients will aid in the prevention of diagnostic delays. If there is diagnostic uncertainty, clinicians and patients can refer to the flowchart below.
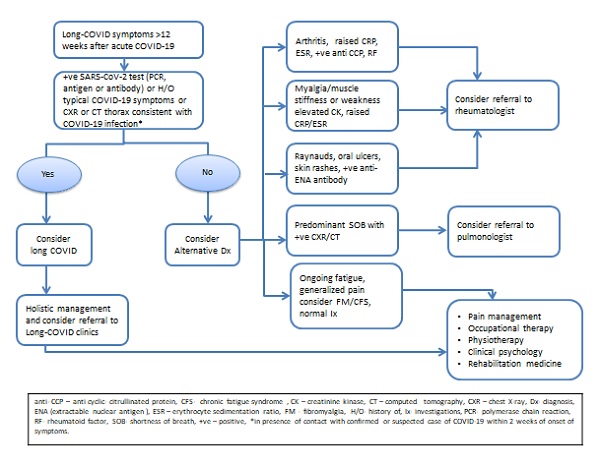
Fig. 2 Flowchart of the management of a patient presenting with long COVID. (anti-CCP anticyclic-citrullinated protein, CFS chronic fatigue syndrome, CK creatinine kinase, CT computed tomography, CXR chest X-ray, Dx diagnosis, ENA extractable nuclear antigen, ESR erythrocyte sedimentation ratio, FM fibromyalgia, H/O history of, Ix investigation, PCR polymerase chain reaction, RF rheumatoid factor, SOB shortness of breath,+ve positive, *in presence of contact with confirmed or suspected COVID-19 within 2 weeks of onset symptoms.)

Dr. Arvind Nune, MBBCh, MSc, MRCP, is a clinician, a teacher and a researcher. He is a practicing consultant Rheumatologist and General Physician in the United Kingdom. His undergraduate studies were in India. Research interests are ‘infection and inflammation’ and he has published several peer-reviewed articles in international journals on rheumatology care delivery during the COVID-19, the emergence of new rheumatic diseases following SARS-CoV2 infection and vaccination, and long COVID. He published the first case of the multisystem inflammatory syndrome (MIS-V) in an adult patient who was infection naïve following the SARS-CoV-2 vaccination and was one of the first researchers to study the incidence and predictors of long COVID in hospitalised patients 9 months after their hospital discharge.
References:
- World Health Organisation (WHO) (2021) A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. Available at https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_con… Accessed 25/10/2021
- ONS 2022. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK. 3 February 2022. [Cited 2022 February 14]. Available from https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare…
- National Institute for Health and Care Excellence. NICE guideline [NG188]. COVID-19 rapid guideline: managing the long-term effects of COVID-19. Published: 18 December 2020 Last updated: 11 November 2021. Overview | COVID-19 rapid guideline: managing the long-term effects of COVID-19 | Guidance | NICE (Accessed 21 March 2022).
- Nune A, Durkowski V, Titman A, Gupta L, Hadzhiivanov M, Ahmed A, Musat C, Sapkota HR. Incidence and risk factors of long COVID in the UK: a single-centre observational study. J R Coll Physicians Edinb. 2021 Dec;51(4):338-343. doi: 10.4997/JRCPE.2021.405. PMID: 34882130.
- Mental Health in the times of COVID-19 Pandemic – Ministry Of Health And Family Welfare (MOHFW). Available from https://www.mohfw.gov.in/pdf/COVID19Final2020ForOnline9July2020.pdf (Accessed 21 March 2022)
- Boglione L, Meli G, Poletti F, Rostagno R, Moglia R, Cantone M, et al. Risk factors and incidence of long-COVID syndrome in hospitalized patients: does remdesivir have a protective effect? QJM. 2022;114(12):865-871
- Sapkota HR, Nune A. Long COVID from rheumatology perspective - a narrative review. Clin Rheumatol. 2022 Feb;41(2):337-348. doi: 10.1007/s10067-021-06001-1. Epub 2021 Nov 30. PMID: 34845562; PMCID: PMC8629735.