Cancer therapies such as Chemotherapy, Radiation and Surgery to the head and neck area as well as Bone Marrow Transplantation can cause various oral complications and dental issues like caries, fungal or bacterial infections, bleeding gums, loss of teeth, dry mouth, oral ulcers, etc. To minimize these complications, a thorough oral assessment before, during and after the completion of treatment is imperative. Dr. Meghana Maruthi guides us through these care pathways that all cancer patients should be aware of and avail when necessary.
1. What is Dental Oncology? Who should avail of it?
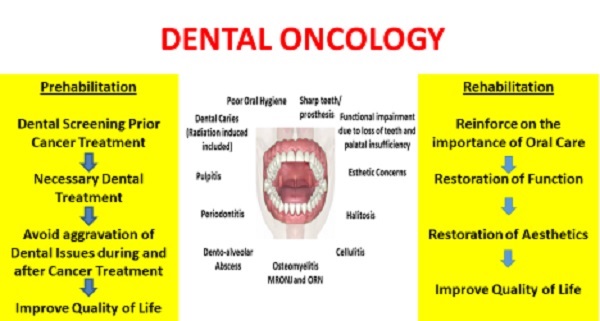
Dental Oncology is a super-specialty in dentistry that deals with meeting the oro-dental needs of all types of cancer patients to improve their quality of life. Dental Oncologists are dentists who are trained to particularly manage cancer patients as they are aware of the cancer treatments and their side-effects. Routine dental procedures such as cleaning, filling, root canal treatment, coronoplasty (blunting and smoothening the teeth cusps),extraction and replacement of teeth along with maxillofacial prosthetics collectively known as prosthodontic rehabilitation are included in Dental Oncology services.
Prehabilitation is currently a trending topic among all rehabilitation physicians which highlights the importance of sensitization, prevention and minimization of the side effects of cancer treatment by prior assessments. It also reduces hospital stay and the financial burden of rehabilitation. Rehabilitation includes restoration of physical, mental and social health of the patient. The following patients should avail dental oncology services prior (prehabilitation), during and after (rehabilitation):
- Surgery in the head and neck region
- Chemotherapy, especially those who are on antiangiogenic medication such as bisphosphonates (Zolendronic acid and others) and Denusumab (irrespective of the tumor site)
- Radiotherapy to the head and neck region
- Bone Marrow Transplantation
- Organ Transplantation
- Immunosuppressive Therapy
- Any cancer patient who has an oro-dental problem
Also, every cancer patient should visit the dental oncologist once in three to six months for a routine check-up.
2. What would pre-treatment assessment entail? Is this offered as standard practice to all required patients?
Yes, pre-treatment dental assessment and treatment are offered as a standard practice to all required patients mentioned above. However, most times the patients and their families do not consider it important as they are fighting a bigger battle. Also, the treating oncologists may not want to wait until the patient finishes all essential dental treatments before starting cancer therapy as the tumors may be aggressive in nature. Therefore, we suggest timely follow-ups to contain the slightest chance of dental infections and traumatic injuries.
Pre-treatment oro-dental assessment includes thorough extra-oral (external) and intra-oral (internal) examination. As a part of the extra-oral examination, we assess the facial asymmetry, temporomandibular joint movements (jaw joint), muscles of mastication (muscles which help in chewing), lymph nodes (nodes which contain white blood cells) and sensory and motor assessment of the nerves. Intra-oral examination includes the evaluation of the hard and soft tissues. Firstly, the mouth opening is assessed as most patients diagnosed with oral cancer and who have received treatment for it may have limited mouth opening making their intra-oral assessment difficult.
Hard tissue includes the teeth and jaws. We look for infections caused by decayed, loose and partially impacted teeth.We use a few indices to assess how susceptible the patient is to teeth decay and their oral hygiene status. We assess sharp teeth which can potentially cause traumatic ulcers.We make a note of the missing teeth and the need for prosthodontic rehabilitation. We also look for exposed bones with/without disease in the jaws(osteonecrosis due to radiation or chemotherapy) and soft tissue abnormalities.A full mouth intra-oral periapical radiographs and/or an orthopantomograph should be advised which will help us in maintaining records and better treatment planning. It is mandatory to thoroughly clean the oral cavity and apply fluoride gel/varnish to the teeth after the initial assessment. This is followed by elimination of all sharp and potential infectious teeth with appropriate dental treatment. Above all this, the patient needs to be educated and motivated about oral hygiene practices every single time he/she visits us.
3. Who is responsible for a patient's oral care?
The patient is primarily responsible to take care of their basic oral hygiene as long as their sense of vision and dexterity is adequate. Dental Oncologists, Dentists, Oncologists, Nurses and Care takers are held equally responsible during various phases of the patients’ treatments.
4. What rehab advice can you give for muscular side effects affecting chewing, swallowing, speech etc.?
Stiffening of the muscles of the head and neck region causes difficulty in opening the mouth (trismus), mastication (chewing), swallowing, speech and can restrict neck and shoulder movements. Depending on the cause and severity of the trismus, it would be ideal to treat it with a multidisciplinary approach and involve the Surgical Oncologist, Speech and Swallow Pathologist, Physiotherapist, Nutritionist, Psycho-oncologist, Integrative Oncologist and Yoga therapist as well. A more conservative approach will involve oro-motor exercises as listed below:
- Forceful opening and closing of the lower jaw using stacked wooden tongue blades/ice cream sticks or a mechanical jaw opening device, example: Heisters or Orabite.
- Moving the lower jaw sideways, front (protrusion) and back (retraction).
- Blowing a balloon or simple cheek blowing exercises.
- Tongue protrusion, lateral movements, rolling and extension to the palate.
- “Ah” sound to be produced to improve the soft palate movement/uvula movement.
- Vocal exercises to improve speech.
- Slow and steady practices of swallowing ones’ own saliva first followed by thin liquids, thick liquids, semi-solids and solids in the course of time.
If trismus is severe and debilitating, the surgical oncologist may consider bilateral coronoidectomy followed by aggressive physiotherapy to improve the mouth opening.
When the patient does not receive adequate nutrition through the oral cavity, nutritionist and oncologists may advice for a Ryle’s tube insertion (feeds given through the nose) or Percutaneous Endoscopic Gastrostomy tube insertion (feeds given directly to the stomach).
5. When is it ideal for extraction of teeth in patients who visit you prior surgery and radiotherapy to the head and neck region, bone marrow transplant, organ transplant, and antiangiogenic chemotherapy?
Extractions should ideally be done 10 to 21 daysprior to the beginning of cancer therapy or at the time of surgery to avoid the risks of delayed wound healing and bone infection (Osteoradionecrosis (ORN) and medication related osteonecrosis of the jaw (MRONJ)).
6. When is it ideal for extraction of teeth in patients who have received radiation in the head and neck region and undergone other cancer therapies?
Extraction should only be considered after careful evaluation. Extremely mobile periodontally compromised teeth can be safely removed with minimal risk of developing ORN and MRONJ.
There are suggestions that a latent period of at least 6 months to 1 year should be provided for those who have undergone radiation to the head and neck region. However, it varies as per the institutional protocols. Complete blood count and prothrombin time should be in normal limits and the co-morbid state should be under control to undergo extraction of tooth/teeth under high coverage antibiotics.
Those patients who are on antiangiogenic and immunosuppressive drugs need to be carefully evaluated and taken up for extraction since these medications have long term effects.
7. What oral hygiene instructions are to be followed by the patients?
Below are the general oral hygiene Instructions which needs to be followed by the patient:
- Brush teeth in a vertical or circular motion with a soft bristle brush 2–3 times a day for 2–3 min. In case of limited mouth opening, use a baby brush or a finger brush.
- Use a fluoride toothpaste with a mild taste, flavouring may irritate the mouth, (especially mint, cinnamon and clove flavoured toothpastes).
- Rinse the toothbrush in hot water every 10–30 seconds to soften the bristle if needed.
- Use antibacterial mouth rinse as prescribed by your dentist.
- Warm Salt-Soda Water Rinses – Do it every 2 hours to decrease soreness in the mouth. To prepare the rinse dissolve ¼ teaspoon of salt and ¼ teaspoon of baking soda in 1 glass of water.
- Use a gauze to clean any residue inside the mouth over gums and tongue. If the patient or the attender is unable to do it, kindly seek help from the professionals.
- Use Floss or Waterpik to clean the areas between the teeth. Do not use toothpick/ safety pin/ needle.
- Use lip care products such as plain petroleum jelly to prevent drying and cracking.
- Visit the dentist with prior appointment once in three to six months.
Also, some of the common issues that patients face and how it can be avoided are stated below:
Dental Caries/Tooth Decay: It can be prevented by good oral hygiene practices, low sugar diet, fluoride therapy and pit and fissure sealants. Dental caries in the initial phases can be treated with a filling, as it advances patient will have to undergo root canal treatment followed by cap/crown or extraction of the tooth.
Mucositis: To minimize the severity of mucositis one must follow good oral hygiene practice, undergo oral prophylaxis and elimination of any trauma causing agents such as sharp tooth/teeth and ill-fitting prosthesis/dentures must be eliminated prior to the beginning of chemotherapy and radiotherapy (specific to the head and neck region). If the patient has a history of bruxism, customized soft occlusal guards must be given. During chemotherapy and radiotherapy, the patient should be well hydrated and rinse the mouth with warm salt-soda water to maintain the pH of the saliva and minimize the bacterial colonization.
Fungal and Viral Infections: Cancer therapy inevitably causes immunosuppression which leads to infections. However, the chance and severity of these infections can be minimized by following the above mentioned oral hygiene instructions correctly.Patient is expected to report to the treating oncologist immediately when he or she has any symptom of infection so that appropriate antibiotic/antifungal/antiviral regimen can be started. Delay in reporting may lead to sepsis and can be life threatening.
Xerostomia/Dry Mouth:With advanced treatment modalities such as Intensity Modulated Radiation Therapy (IMRT), the incidence of xerostomia is reduced. For those who are symptomatic, we recommend frequent sipping of water to cleanse the mouth and keep it moist. Artificial saliva in the form of gels, sprays and mouth rinses can be used by the patient whenever required. Based on our sialometric assessment we may advise a few stimulants which are well tolerated by the patients to increase their salivary flow such as sugarless chewing gum, paraffin wax, etc. which will minimize the incidence of radiation caries as well.
Instructions for Denture Wearers:
- All denture wearers should brush all the surfaces of the denture with mild soap and brush once daily and clean their oral cavity with finger or gauze to remove soft tissue plaque/residue.
- Remove and rinse the denture with water after every meal.
- Remove the denture at night and keep it in a container containing water.
- Discontinue wearing the denture if you develop any denture sore or ulcers and report to the dentist/dental oncologist.
- Discontinue wearing dentures if they are ill-fitting and report to the dentist/dental oncologist.
Ulcers and Blisters: There are various etiological factors for a cancer patient to develop oral ulcers and blisters. The most common one being cancer therapy itself. Most ulcers are the manifestation of mucositis and its severity can be minimized as mentioned above under mucositis. Canker sores/Apthous ulcers are mostly stress related and are associated with nutritional deficiencies. Therefore, adequate nutrition is essential to contain all complications of cancer therapy.
Bleeding Gums and Periodontal Disease: Poor oral hygiene leads to periodontal diseases and a higher bleeding index. This can be prevented by instructions given above. Co-morbid condition such as diabetes is considered as a risk factor for periodontal disease. In such cases, the main condition needs to addressed prior to any dental intervention.
To conclude, oro-dental assessment and prompt treatment is important to provide a better quality of life to cancer patients.It nourishes the patient physically, mentally and socially by minimizing the chance of infection and by maintaining oral functions and aesthetics.