
Vertigo and dizziness, a common complaint among older adults greatly impacts daily life and is a major risk factor for falls with severe long term health consequences. Dr Aditi Sinha, an ENT Specialist from Mumbai addresses how vertigo is treated, what happens if left untreated and whether or not vertigo can be reversed.
The most common treatments for vertigo include:
Home remedies
The majority of home remedies are designed to prevent or reduce the risk for a vertigo episode, but some can be used when the disorientation begins. These include:
- avoiding caffeine, tobacco, and alcohol
- staying hydrated
- taking multivitamin and mineral supplements.
- yoga, meditation and other relaxation techniques
Medications
Some medications may help stop severe vertigo episodes. The most commonly prescribed medications for vertigo are:
- anti-nausea medicines, such as promethazine and prochlorperazine
- sedative medicines, such as diazepam
- antihistamines, such as diphenhydramine, Cinnarizine, Betahistine
These medicines may be administered by mouth, patch, suppository, or IV. Both over-the-counter (OTC) and prescription options are available.
Physical therapy maneuvers
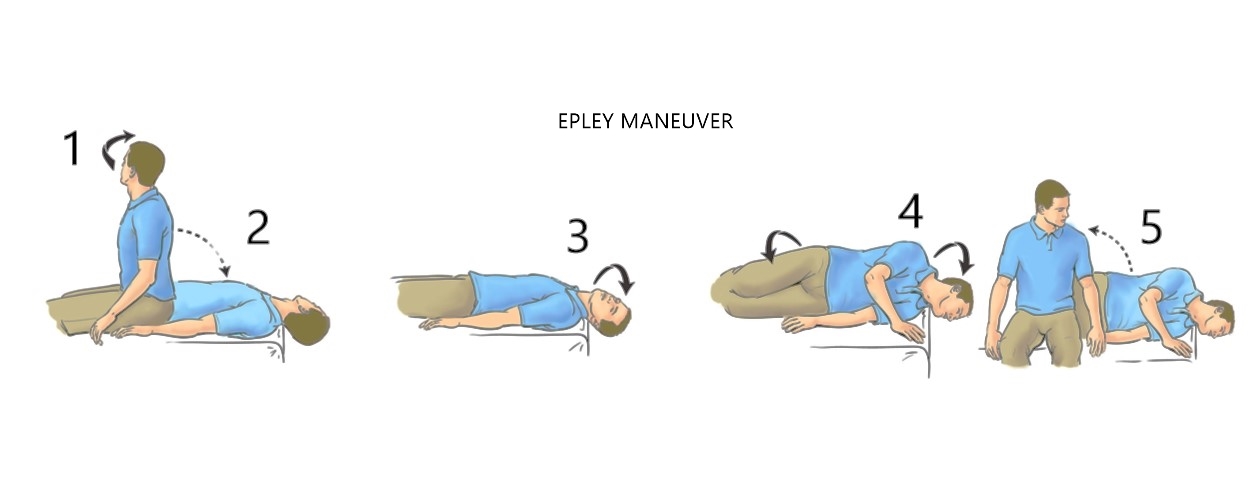
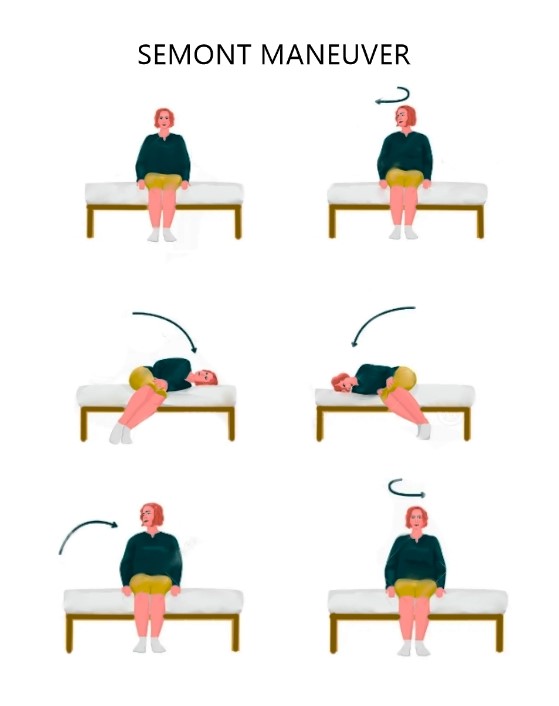
Two main physical therapy maneuvers are used to treat symptoms of vertigo. Your doctor will work with you to learn the proper technique so you can perform them correctly. These maneuvers include:
- Modified Epley maneuvers. The Epley maneuver is a type of treatment that uses head and body movements to encourage the inner ear to reabsorb any matter that’s floating in the inner ear and causing vertigo. The relief can be immediate, or it may take several days.
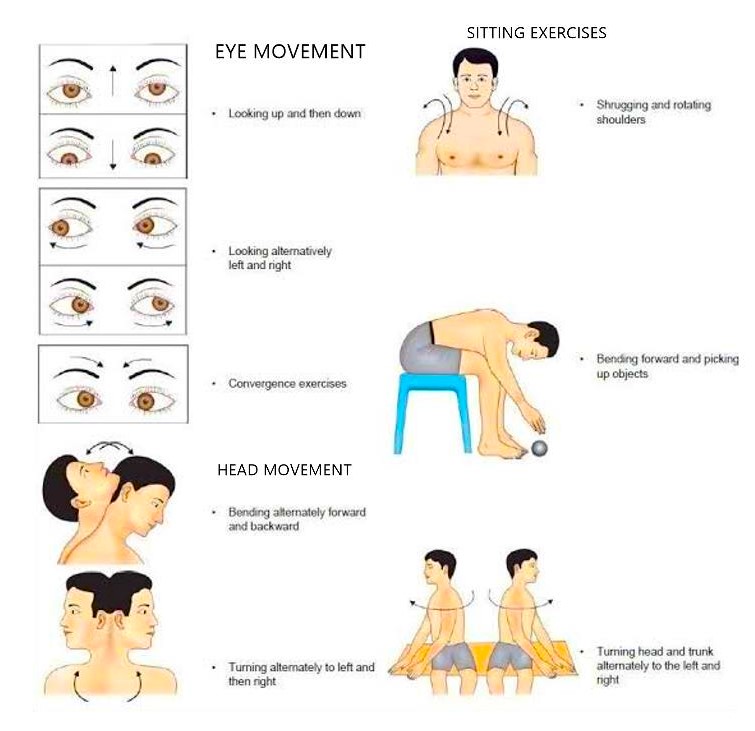
- Vestibular rehabilitation exercises. Moving your head and body when you’re experiencing a vertigo episode may feel too difficult. Your doctor can teach you rehabilitation exercises that can help your brain adjust to the changes in the inner ear. These balancing techniques will help your eyes and other senses learn to cope with the disorientation. The Semont manoeuvre is a set of simple movements that can provide relief from dizziness for people with BPPV.
Vertigo if left untreated can become chronic, unresponsive to treatment and an interference to routine life. It can lead to falls and its medical/surgical implications, lack of confidence, social isolation anxiety, depression.
You should seek emergency medical help if you experience vertigo with any of the following RED FLAG signs:
- a severe headache
- a high fever
- weakness in your arms or legs
- inability or trouble walking, speaking, hearing, or seeing
- passing out
- chest pain
Vertigo will often go away by itself, but if it is severe or happens regularly then it's important to see a doctor. An ENT consultant will be able to find out why it is happening and recommend treatments to relieve or manage your symptoms. The best approach will depend on the cause of your vertigo. After diagnosis, vertigo can be managed efficiently even if not 100% reversed. Symptoms may become episodic, fewer and far between with less intensity of discomfort.
What are your recommendations for management of vertigo?
I feel that, vertigo represents one of the most common problems in the elderly and is also a serious condition, often leading to increased morbidity and mortality. It’s important to talk with your doctor any time you experience vertigo. They can work with you to understand the underlying cause and find treatments that can both prevent vertigo attacks and ease them if and when they occur. Fortunately, most of the underlying causes of peripheral vertigo aren’t serious. They can be treated easily, which will eliminate vertigo episodes. If the underlying cause can’t be treated, your doctor can work with you to reduce disorientation and hopefully prevent future complications.
Audio-vestibular disorders, and among these BPPV, represent the most frequent cause of vertigo; a greater awareness of these conditions should be advocated among specialists dealing with patients of this age group. Moreover, doctors should always carefully investigate these patients, in order to identify the different factors underlying this condition and the eventual concurrent pathologies.
How can daily routines and quality of life be improved for the senior patients?
The most serious consequence of vertigo is the increased risk of falling. For older adults, this is especially important because they have a higher risk of injuries, such as head trauma, bone fractures, and soft tissue damage. These injuries could lead to long-term disability.
To prevent falls, consider the following strategies:
- Stay physically active for improved strength and balance.
- Install handrails in your home.
- Stand up slowly, and always keep a chair nearby.
- Use an assistive device, such as a cane or walker.
- Fasten all carpets and rugs to the floor.
- Ensure you have good lighting at home.
- Prepare food while seated.
- Use a “reach stick” to get items on high shelves.
- Wear non-skid, rubber-soled shoes.
- Talk with your doctor if a new medication is making you dizzy.
Any time you get vertigo, you are at an increased risk of falling. By noticing when you may experience attacks, you can take steps to stay safe in the event of a fall.
Improving activities of daily living
The ultimate goal of vestibular recovery should be to enable the patient to return to all of his or her normal activities of daily living. Therefore, VRT and vertigo treatment is not considered to be complete until the patient has returned to normal work or is satisfactorily resettled. Patients who are unable to return to their normal work and in whom the disability is likely to last at least 6 months are considered to be disabled.
To achieve the final goal of vestibular recovery, the exercise is integrated into normal activities such as walking, rather than being performed with the patient sitting or standing quietly. Various games can be introduced to reduce the monotony of purely remedial exercises. Patients who are gradually and safely exposed to a wide variety of sensory and motor environments are teaching their nervous systems to identify strategies to accomplish functional goals. All patients who receive customized VRT programs are also provided with suggestions for a general exercise program that is suited to their age, health, and interests. For most, this would at least involve a graduated walking program. For many, a more strenuous program is suggested that may include jogging, walking on a treadmill, doing aerobic exercises, or bicycling. Activities that involve coordinated eye, head, and body movements such as golf, bowling, handball, or racquet sports may be appropriate. Swimming should be approached cautiously because of the disorientation experienced by many vestibular patients in the relative weightlessness of the aquatic environment. Older adults who talk as they walk with assistive devices are more likely to fall than those who do not talk as they walk. Therefore, older patients should be instructed that when a conversation is started they should stop walking in order to prevent falling. If rapid head movements cause imbalance, the patients should be advised not to drive.
Reassurance and/or counseling with rehabilitation and regular follow ups with the treating doctor and/or team are vital in recovery and maintaining the life routine.
Chronic vertigo may lead to psychological issues of fear and anxiety, how are such patients managed?
Anxiety and vertigo have a reciprocal relationship in which anxiety can cause vertigo/dizziness, and dizziness can cause anxiety. Research has shown that in many cases, vertigo/dizziness and anxiety go hand-in-hand, which can sometimes create a loop of chronic symptoms. By treating the underlying cause whether physical or psychological you can relieve the symptoms of dizziness and improve your overall quality of life.
Vestibular disorders, also known as inner ear disorders, are also linked to increased anxiety, especially in conditions that cause severe disability. In some cases, having a vestibular disorder that causes chronic episodes of dizziness or vertigo may even increase the risk of developing an anxiety disorder.
BPPV
Researchers have found that those with anxiety disorders were more than twice as likely to develop BPPV. Researchers also observed an increased risk of developing BPPV if the person was female or had cerebrovascular disease.
In a more recent study Trusted Source, researchers investigated the correlation between anxiety, disability, and quality of life in participants with vertigo. Results of the study indicated that almost all participants experienced some level of anxiety, ranging from mild to severe. However, people whose dizziness was more severe were found to have increased anxiety and disability and lower quality of life. Stress hormones, which include cortisol, histamines, and other compounds that are released during the stress response, have an impact on vestibular function.
As for the correlation between balance disorders and anxiety, the National Institute of Mental Health (NIMH)Trusted Source explains that having a chronic illness is linked to an increased risk of developing a mental health disorder. When conditions like BPPV and vestibular migraine make it difficult to function in everyday life, it can cause an increase in symptoms of anxiety and depression.
Frequent dizziness tends to lead to increased anxiety, while chronic anxiety often causes chronic dizziness. Sometimes, this relationship can create a vicious circle that is hard to break without taking steps to relieve symptoms.
Making lifestyle changes, such as eating a well-balanced diet, practicing relaxation techniques, and getting professional help can help improve quality of life in people with both anxiety and vestibular disorders.
- Psychotherapy techniques such as cognitive behavioral therapy (CBT) have a long history of success in treating anxiety disorders. Increasing self-awareness of anxiety and learning coping skills can help reduce some of the symptoms of chronic anxiety.
- Medications. Antidepressants are the most commonly prescribed medication for both depression and anxiety disorders. Most times, medications are used in combination with psychotherapy to produce long-term reductions in anxious feelings and symptoms.
- Lifestyle changes. In addition to therapy and medications, relaxation techniques can be an essential part of managing daily stress levels. Meditation, yoga, and gentle exercise are just a few ways to reduce the everyday symptoms of anxiety and stress.
What prosthetic devices are available to improve vertigo?
The UW/Nucleus vestibular implant is a multistage device that can function as a pacemaker or a sensor-based prosthesis. It's akin to a modified cochlear implant.
The vestibular implant consists of motion sensors rigidly fixed to the patient's head and of electronic components (processor and stimulator) that translate the received motion information into electrical signals transmitted to the brain via electrodes implanted in the vicinity of vestibular nerve endings.
Given the collateral damage to hearing observed in some of the implanted patients and because other implants have been done in patients with profound deafness (Guyot and Perez-Fornos, 2019), it is possible to conclude that, to date, the indication for the vestibular implant must be limited to patients with unilateral deafness. In the future, electrode improvement, stimulation selectivity, surgical techniques (Handler et al., 2017; van de Berg et al., 2017b; Schier et al., 2018), and better methods of electrode fixation will surely expand the possibility of vestibular implantation in subjects, producing no or mild auditory damage.
What is Vestibular rehabilitation? Is it routinely available in India?
Vestibular rehabilitation therapy (VRT) is an exercise-based treatment program designed to promote vestibular adaptation and substitution. The goals of VRT are:
- to enhance gaze stability,
- to enhance postural stability,
- to improve vertigo and,
- to improve activities of daily living.
The exercises for vestibular rehabilitation can be categorized into two types:
1) Physical therapy for vestibular hypofunction and 2) Canalith repositioning therapy for benign paroxysmal positional vertigo (BPPV).
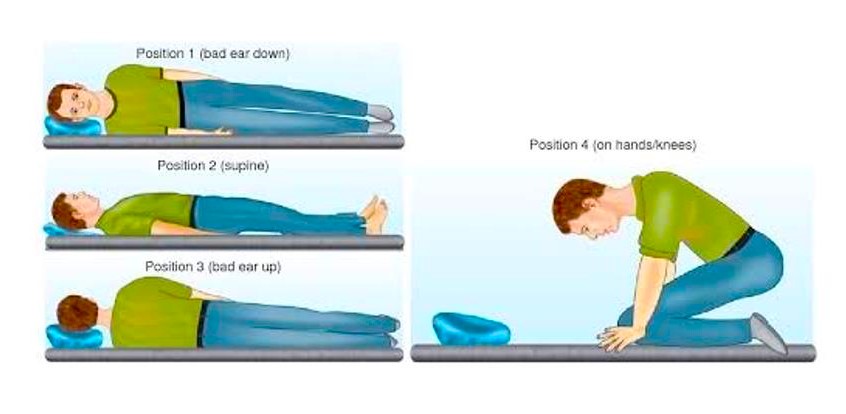
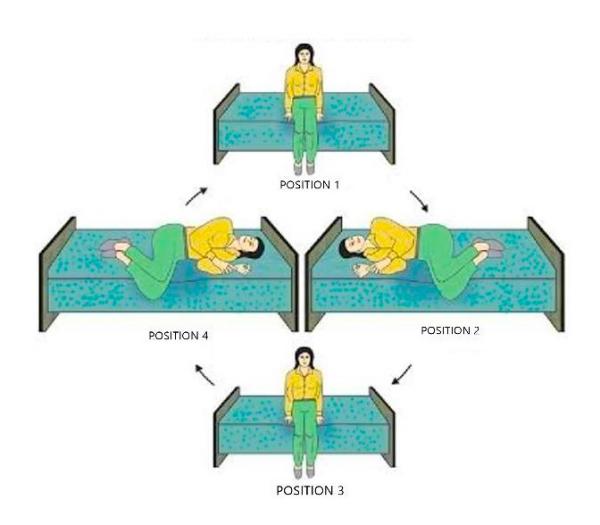
The key exercises for VRT are head-eye movements with various body postures and activities, and maintaining balance with a reduced support base with various orientations of the head and trunk, while performing various upper-extremity tasks, repeating the movements provoking vertigo, and exposing patients gradually to various sensory and motor environments. VRT is indicated for any stable but poorly compensated vestibular lesion, regardless of the patient's age, the cause, and symptom duration and intensity. As long as exercises are performed several times every day, even brief periods of exercise are sufficient to facilitate vestibular recovery.
In older adults with symptoms of dizziness and no documented vestibular deficits, the addition of vestibular-specific gaze stability exercises to standard balance rehabilitation results in a greater reduction in fall risk.
Exercise frequency and duration:
Patients should perform exercise for gaze stability four to five times daily for a total of 20-40 minutes/day, plus 20 minutes/day of balance and gait exercises. Each exercise may be performed at least twice per day, beginning with five repetitions of each and increasing to ten repetitions.
How to progress
- Follow-up visits
Patients are typically seen once every 1-2 weeks and are provided with a specific daily home exercise program. During each visit the therapist addresses the specific problems and goals of the individual patient. Simple easy to perform exercises are taught and exercise charts are given for home reference.Safety is a major concern, so that therapists should always monitor patients during a treatment session. Now, VRT is readily available and accessible in India at all major hospitals with ENT and Audiology departments.
It is offered at the said department or in the Physiotherapy & Neuro rehabilitation department of the hospital.Standalone big Physiotherapy establishments and chains across India offer these services like routine Physiotherapy sessions in metros and most tier 1 and tier 2 cities.

Dr. Aditi Sinha is an ENT Specialist- Head & Neck Surgeon with over a decade of clinical experience across leading hospitals in Mumbai. She currently practices at Masina Hospital (Byculla) Inlaks General Hospital(Chembur), Dhanwantari Hospital & Research Center(Dadar) and Sanghvi JB Trust Clinic & Hospital(Matunga), Mumbai.
Her chief areas of clinical interest are deafness, vertigo and allergy management.
References:
- Prevalence and etiology of vertigo in adult rural population. Abrol R, Nehru VI, Venkatramana Y. Indian J Otolaryngol Head Neck Surg. 2001;53:32–36.
- Muncie HL, Sirmans SM, James E. Dizziness: Approach to Evaluation and Management. Am Fam Physician. 2017 Feb 01;95(3):154-162. [PubMed]
- Kerber KA, Newman-Toker DE. Misdiagnosing Dizzy Patients: Common Pitfalls in Clinical Practice. Neurol Clin. 2015 Aug;33(3):565-75, viii. [PMC free article] [PubMed]
- Grill E, Strupp M, Müller M, Jahn K. Health services utilization of patients with vertigo in primary care: a retrospective cohort study. J Neurol. 2014 Aug;261(8):1492-8. [PubMed]
- Parker IG, Hartel G, Paratz J, Choy NL, Rahmann A. A Systematic Review of the Reported Proportions of Diagnoses for Dizziness and Vertigo. Otol Neurotol. 2019 Jan;40(1):6-15. [PubMed]
- Hornibrook J. Benign Paroxysmal Positional Vertigo (BPPV): History, Pathophysiology, Office Treatment and Future Directions. Int J Otolaryngol. 2011;2011:835671. [PMC free article] [PubMed]
- Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ. 2003 Sep 30;169(7):681-93. [PMC free article] [PubMed]
- Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000 May;122(5):630-4. [PubMed]
- von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007 Jul;78(7):710-5. [PMC free article] [PubMed]42.
- Fujino A, Tokumasu K, Yosio S, Naganuma H, Yoneda S, Nakamura K. Vestibular training for benign paroxysmal positional vertigo. Its efficacy in comparison with antivertigo drugs. Arch Otolaryngol Head Neck Surg. 1994 May;120(5):497-504. [PubMed]43.
- Pérez-Vázquez P, Franco-Gutiérrez V, Soto-Varela A, Amor-Dorado JC, Martín-Sanz E, Oliva-Domínguez M, Lopez-Escamez JA. Practice Guidelines for the Diagnosis and Management of Benign Paroxysmal Positional Vertigo Otoneurology Committee of Spanish Otorhinolaryngology and Head and Neck Surgery Consensus Document. Acta Otorrinolaringol Esp (Engl Ed). 2018 Nov-Dec;69(6):345-366. [PubMed]






