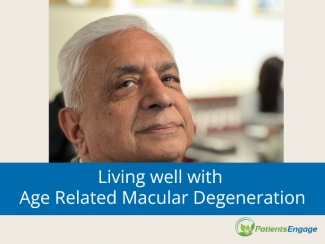
But often overlooked, says Porrselvi A.P. a cognitive and psychosocial interventions specialist. Here, she offers a case study and practical strategies to guide you back to normal life.
The patient: Mrs. K, a 67-year-old woman had a stroke in the left side of her brain in September last year.
Her condition: Mrs K was referred for cognitive and psychological evaluation following complaints of social withdrawal, memory disturbances and increased irritability. She also had sleep disturbances. She preferred to just lie down throughout the day or spend the entire day in front of the TV, though she never paid attention or followed any show on the TV. She refused to take her medicines or food and her caregiver’s main complaint was that Mrs. K was very irritable and verbally abused her when given her tablets.
A formerly very independent woman, she still preferred to do all her Activities of Daily Living (ADLs) herself and usually accomplished the tasks, but she was slower in her activities now which may be explained by the weakness on her right side due to the stroke. She was pre-occupied with her health condition. She felt she was getting incontinent and was concerned about it. She said she felt lonely frequently because her grown up grandchildren were away in college though she had previously lived by herself till she had the stroke.
Diagnosis: On psychological assessment, it was found that Mrs K had moderate to severe clinical depression. She was also anxious about her health though she did not fulfil the criteria for an anxiety disorder.
On cognitive evaluation, it was found that she had significant impairment in the cognitive domain of attention. That is, she was not able to focus on what was required and relevant to her while drowning out the other stimuli she was receiving from her environment. Also, she was not able to pay attention to a stimulus for long. This can explain why she was unable to follow conversations which, when coupled with the depression she was experiencing, was making her socially withdrawn, sad and lonely.
Post-stroke depression is common. It has been seen that strokes cause depression in patients due to the biochemical changes that the brain goes through. It is much more common than reported but is seldom paid attention to because it is taken for granted that the patient is just morose after their hospital stay and due to the losses and impairments they face post-stroke. Post-stroke depression is more common among stroke survivors whose brains are affected on the left side.
Depression affects the physical, functional and cognitive recovery of the person. It causes social withdrawal and is associated with increased mortality. The development and severity of Post-Stroke Depression depends on multiple factors like lesion location, presence and extent of functional impairments, amount of social dependence, severity of cognitive impairment, ability to return to prior occupation, stroke onset etc.
So what was troubling Mrs K?
1. Inability to understand her medical prescription was making her angry. It was found during the counselling session that she did not understand her medical prescription which was contributing to the agitation when she was given her tablets by her caregiver. She could only understand that there were 9 tablet names on her prescription while her caregiver was giving her 7 in the morning, 4 in the afternoon, 2 before her meals and 6 at night.
How we managed this problem: One of the rehabilitation goals framed for her was to help her understand the prescription and then building strategies to help her follow the differential dosage pattern she had to follow through the day. She was also given therapy to understand that her caregiver was not trying to avoid giving her medicines she needs.
2. Depression
How we managed this: This was addressed by patient education and counselling in addition to the medications prescribed by the neurologist. Problem solving therapy was used with relaxation techniques and some elements of cognitive behavioural therapy. For example, we helped to build a routine to her day, thereby structuring it and helping her be more active. Exercise and a balanced diet were built into her schedule. Also, the patient education which happens during the course of the sessions gives the patient a better understanding of their condition and what they need to do to feel better. This education is given taking into account the cognitive impairments that the patient may experience.
3. Inability to concentrate
How we managed this: Cognitive Rehabilitation was done to address the deficits in attention mainly by teaching external strategies, process training and functional activities training.
External strategies are gadgets, techniques that can be used to help overcome deficits, eg making a shopping list for someone who has memory or attention deficits.
Process training works on the basic neural circuitry by doing tasks that are known to include the processes like attention or memory and thereby, strengthening the circuitry. It is like working out the muscles you want to build.
Functional activities training works by identifying activities that the patient finds challenging and then integrating the strategies learnt and process training done during the rehabilitation sessions to help the patient accomplish the activities they need to accomplish. E.g. building a shopping list, then rehearsing the list, so that eventually the patient will be able to buy at least all the common things she shops for without a problem.
Mrs. K was also given patient education tasks to understand her deficits and to help her anticipate problems she may have with doing some tasks. For example, she was taught how to avoid drifting off during conversations with her family due to the attention deficits she had. The caregiver was also advised to call out her name periodically and include her in the conversation by asking her what she thought.
Soon she learnt how to avoid running into those problems by using the external strategies.
4. Poor communication between Mrs K and her caregiver
How we managed this: Caregiver education and counselling was done. The rehabilitation goals were framed in a manner so that the caregiver could take some time off for herself while not compromising on the care received by Mrs. K. Mrs. K was also made to understand how she can help around at home with every day chores and also help people care for her better. For example, she was made to understand why she should not lock the bathroom door from the inside or why she can’t work near the fire in the kitchen. The caregiver was educated on how to communicate with Mrs. K in view of her deficits. For example, the caregiver was made to understand why Mrs. K gets frustrated with too much information given (e.g. X is marrying Y who is T’s son-in law’s brother); why she does not get sarcasm, jokes etc. and gets offended and tearful.
Outcome
From the day of assessment to the day of the last review, we spent 5 months with her with about 8 sessions in varying intervals across these months. During our last review, she had recovered from depression though she sometimes reported to be sad and irritable, she also said she had learnt to distract herself and “get going”. She stopped being tearful and learnt to Skype her grandchildren whenever she missed them. She did regular exercise and was more open to accepting physiotherapy. The caregiver was most happy for the end of the “medicine time drama”. The deficits in her attention remain though she is able to follow conversations that are addressed to her and her “memory lapses” are not as pronounced as before. She is easily tired and prefers to lie down but her daytime sleeping has reduced and she sleeps better at night.