
Dr Sujeet Rajan, a highly reputed Pulmonologist spoke on ILD (Interstitial Lung Disease) and its management in Scleroderma at the Sclerocon e-conference held in June 2023. In simple terms, Dr Rajan explains what happens during ILD and Pulmonary Hypertension and benefits of preventive along with rehabilitative therapy in Scleroderma Lung disease.
Systemic sclerosis or Scleroderma can affect the lung in several ways. What we need to worry about in Scleroderma is pulmonary hypertension, interstitial lung disease, renal failure and reflux (GERD).
There are 3 parts in the lung that we must know to understand what is happening in because sometimes you have an airway problem, sometimes you have a structure problem and sometimes you have a problem in the lung vessels which is the pulmonary arteries. So, these three components of a lung are different and need to be understood in different perspectives.
1. The Airways are the simplest part of the lung. They are balanced, bilateral and branched out into the lungs and look like trees turned upside down. They are rarely involved in Scleroderma. In airway diseases such as COPD and Asthma, these branches become narrow and the lungs distend. Such diseases are pretty easy to manage with inhalers.
Full video can be seen at https://www.youtube.com/watch?v=DoUTYfXe7Gw
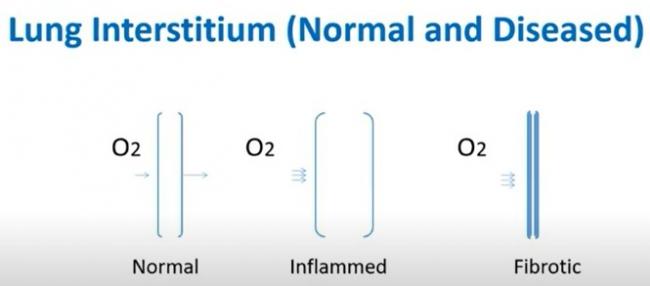
2. Structural or Parenchymal diseases are more difficult to treat. This is what gets affected in Scleroderma. The interstitium is the thin lining inside our lung which transfers oxygen into the blood. The airways just bring the oxygen to the line, so they are conducting mechanism but the transfer into the blood occurs via the interstitium. Therefore, one of the tests to understand the interstitium is called the DLCO, which measures how well this interstitium is functioning. If you've ever done a lung function test, you may have done your DLCO. The area of the interstitium is huge; if you stretch it out, it is as big as a tennis court, so you can imagine how much interstitium we have in our lungs. It can get affected in two ways, one is that it can get swollen, and the other is it can get fibrosed or scarred. Both of these situations cause a problem in getting oxygen into the blood. Inflammation as the middle diagram shows can be potentially reversed but once fibrosis occurs there is still no drug available to reverse that fibrosis. For inflammation you have steroids, azathioprine, mycophenolate and cyclophosphamide that have been tried to reverse the inflammation with decent results. For fibrosis you have now anti-fibrotic drugs available that's slow the progress of the fibrosis. Many people get scared because they hear about a disease called IPF where fibrosis occurs in the lung without a cause, and when it happens without a cause it progresses without a cause and that's dangerous.
Scleroderma lung fibrosis is different in that usually the patients are younger. While IPF happens in older patients, females more than males and affects only the lung. In Scleroderma, other systems also tend to get involved such as the skin, joints and sometimes the pulmonary vessels and the renal system. Autoimmune serology is positive and that's why autoimmune therapies or immunomodulation is given in Scleroderma unlike IPF. IPF progresses much faster than scleroderma so those are the differences. So don't get worried when you read on the internet about IPF and its 2-5 year survival as it does not apply to Scleroderma fibrosis. Only 9% of all the fibrosing lung diseases that I see as a lung physician are patients are Scleroderma. They show the NSIP pattern on the scan, and not UIP pattern which is seen IPF. 40 percent of these Scleroderma lung fibrosis patients have a progressive phenotype and therefore they can progress.
The adverse prognostic factors are:
- diffuse skin involvement less than seven years since the diagnosis
- black race
- the presence of antibodies in the blood
- male sex
- disease extent more than 20 percent on CT with reduced functional vital capacity (FVC) in DLCO.
So these are signs that you need to know to get the fibrosis treated or prevent the progression.
Monitoring ILD in Scleroderma:
- Symptoms: Cough, dyspnea (the breathlessness), skin thickening.
- Examinations to check for crackles and oxygen saturation.
- Lung function testing is extremely important and sometimes done less often than required by rheumatologists. Functional vital capacity or FVC, DLCO on a 6 minute walk test every three to six months, and a high resolution CT scan as and when needed.
The first studies were the SLS I which was done in only one country in the United States and there was no criteria for fibrosis scoring on the scan. Cyclophosphomide was given to a lot of patients, who dropped out due to side effects. Mycophenolate (MMF) was tested here because we needed a longer term option than giving IV cyclophosphamide every three weeks four weeks. Another study was SLS II which basically studied mycophenolate with cyclophosphamide and found that MMF was tolerated better, so many of you may be on mycophenolate for that reason. However, neither mycophenolate or cyclophosphamide is approved for Scleroderma. On CT scan, there was no scoring of the fibrosis and you expected vital capacity to improve but it didn't improve and the effect peaked at 21 months. The interest has now been on fibrosis and Scleroderma and that's the area where a respiratory physician gets involved. When you have no fibrosis on your scan your prognosis is very good, whereas even a little fibrosis increases your risk of mortality or the SMR (standardized mortality ratio). Hence, even a small amount of fibrosis is worse than no fibrosis. As that fibrosis extent increases you have a higher risk and therefore the anti-fibrotic drug should start the moment you see fibrosis on the scan. The SENSCIS study was done in 32 countries including India, and that trial showed that an anti-fibrotic drug named Nintedanib actually slowed the decline in vital capacity. This was huge, as there was 44% relative reduction versus placebo. This treatment effect is meaningful because this starts at middle age and so therefore there is smaller annual decline which accumulates over several years. We know that FVC dropping is associated with mortality and this effect is the same whether you have a lot of fibrosis in the lung or minimal fibrosis and so therefore this is an important treatment that we need to understand in patients who are on mycophenolate. So, if the patient was on mycophenolate, the drop in vital capacity was even less, so there's no harm in continuing both these drugs. Hepatotoxicity or liver toxicity could be slightly higher but the studies did not show that it was higher because the way they are toxic to the liver is in different mechanisms.
3. The third part of our lung is the vasculature and all the pulmonary arteries. We've been hearing a lot about Pulmonary hypertension in the last 10 years. About 15 years ago we had a blank slide on treating pulmonary artery hypertension but we now have multiple treatments. Here are the 4 chambers of the heart in a simple table form. Now in the left ventricle, blood pressure is 110 over 80. You need a blood pressure instrument to check the pressure and you know the pressure in your left ventricle which pumps through the aorta to the entire body. The right ventricle is a much smaller chamber, 1/3th the size of the left ventricle and it pumps through the pulmonary artery to the lungs. The lungs oxygenate this blood and returns to the left atrium and down to the left ventricle and then it's pumped to our entire body. The pressure in the right ventricle is 25 over 10 and you cannot measure this pressure with a blood pressure instrument. Echo is one of the best screening tests for this, as you cannot find out this pressure by checking blood pressure or clinically examining the patient. When pulmonary hypertension develops, the right ventricle pressure goes up to 85 over 30 sometimes. A right heart CATH or angiography is required to study the right side of the heart to accurately get this pressure which I would recommend for any patient who is a strong candidate for Pulmonary artery hypertension. When you start feeling giddy in Scleroderma and have blackouts is when that right ventricular pressure goes over the left ventricle pressure. So when the pulmonary artery pressure is higher than the left ventricle then your blood pressure drops then you get those blackouts. You don't want to be diagnosed at that stage but much earlier because you can treat this. The treatments in pulmonary hypertension are those that are exclusive to the disease and patient needs. Both are important but patient needs are more important.


Here are some of the drugs used for PAH, that some of you may be on.
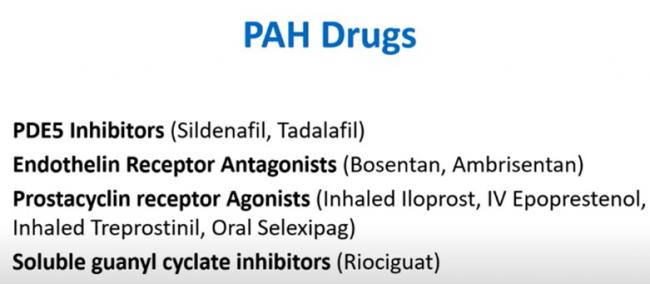
Those who don't have pulmonary hypertension or have digital ulcers will probably need these drugs even if you don't have pulmonary hypertension. One of the landmark trials for this was the Inhaled Treprostinil trial which has now been used in pulmonary hypertension due to ILD. A lot of ILD patients get pulmonary hypertension and this is one of the first approved drugs to treat pulmonary hypertension and ILD, unfortunately not yet available in India.
Preventive and Rehabilitative therapy in Scleroderma Lung disease
Patient’s needs, I find are more important because as the disease advances, there's a lot you need to do.
- Oxygen is a drug and it should be used correctly at rest and on mobility. Some people have a normal oxygen saturation at rest but drop on exercise. Some people drop only at night and you can do a test called the overnight oximetry to check whether you're dropping at night and use oxygen only while sleeping. Use of oxygen should be done correctly. I have seen some prescriptions which say use for one hour in the morning two hours in the night, which makes no sense at all. Know your oxygen saturation at rest and on walking to accurately prescribe.
- Pulmonary Rehab is extremely important here, but under a supervised physiotherapist who understands cardiopulmonary rehabilitation. There are some great physios and there are online cardiopulmonary rehab physios who can teach you how to do this in the best way possible. It should be ideally a physiotherapist who is MPT in cardiopulmonary rehab that's the best type of physio to enrol.
- Management of reflux because of esophageal dilatation is equally important as it can trouble the patients.
- Vaccinations of pneumonia, the annual influenza vaccine and now recently available Herpes zoster vaccine. Vaccinations are critical and often forgotten. One bad attack of flu or Covid can really set you back. A patient with heart failure gets half a dozen drugs prescribed to them the moment they're diagnosed. Two vaccines to prevent respiratory infection are often missed and so you need to ask your doctor whether you should be vaccinated. There are two different types of pneumonia vaccine to be taken one year apart and another booster pneumonia vaccine after the age of 65 and a flu shot quadrivalent southern hemisphere strain for Indian patients once a year. The Zoster vaccine is routinely recommended for the general population above the age of 50 and is even more important to get for the scleroderma patient. It has two doses to be taken 2-6 months apart.
- Supportive and palliative care. Palliative care medicine is often misunderstood as hospice and end-of-life care and is perceived as giving up on the patient. Many doctor/physician colleagues think that palliative care is all about end-of-life care, and this is a huge mistake. We need to understand that palliative care or supportive care as I like to call it, goes hand in hand with the regular treatment and rehab. All this is part of palliative care. You want to have a better quality of life as well with whatever new treatments are available. Your quality of life is as important if not more important! The first author of The Palliative Care Consensus statement in the Lancet wrote “what is worse than chemo in cancer is not having the choice to have chemo.” I think this reflects so much on what patients want. Patients want to choose what they would like to get and so never get forced into doing something by anyone especially your physician. Ask them the questions, so that you get answers that you're comfortable with and if you're not comfortable with it, please do have another discussion with them or go to a physician who's happy to give you the time to discuss these things now and not when emergencies happen. Most of the time we are having these discussions outside in ICU in very sick patients about whether they should be ventilated or given CPR. These should be done in advance. Sometimes relatives tell us “do everything” and I wish more people knew the misery of doing everything. All patients with advanced lung disease should meet our supportive Care Consultants so we manage you as a team because we believe that there's one thing that we can do for a disease, there's another thing we can do to improve the quality of the life of the patient.
-
- Referral for transplant. A lot of patients with pulmonary hypertension and Scleroderma were going for heart & lung transplants but that whole scenario has changed. Very few need to go for transplant because of treatments available now.
What do patients want from a physician?
This was a Yale study where patients were asked what do they want from their doctor and they said:
- A doctor they can trust
- A doctor who is competent
- A doctor who puts their priorities before anything else when they make a management plan
You would be surprised to know that two of these points are not taught very often in our medical colleges. We are taught to be competent doctors but are not taught how to build trust in a patient and how to put the patient's priorities before anything else. I was in taught and I still see this is not being taught barring a few situations where you have great mentors. We are taught so much about disease that we believe when we come out of Medical College all we need to do is cure disease and we forget about the patient in front of us.
When is end-of-life care discussed?
These discussions often happen three days before a patient dies and that is hardly the time that these discussions should happen. The triggers to begin talking about palliative and supportive care are:
- Elderly patients above age of 75
- Patients who are functionally dependent on their families
- Patient-reported minimal physical activity (wheelchair arrival)
- Oxygen dependency on ventilation (BPAP or non-invasive ventilation)
- Hospitalized more than once in the last one year
Shared Decision Making
I'd like to conclude on shared decision making. We have much better drugs for scleroderma than we
have ever had but shared decision making in many diseases now has become a model for clinical practice where the doctor tells you all that is available and you tell them what your priorities are and then you take a shared decision. I would encourage patients to spend that time with doctors discussing what their priorities are so that the best possible decision can be made in their best interests.
Finally, lung involvement in Scleroderma is not always the case but it can happen and it needs attention so protect your lungs in Scleroderma. Be alert! If you're looking at tests to understand Lung and how badly they are affected, you need a good quality scan and a good report. If you don't have a good CT radiologist, you're going to get a poor quality scan and report. We have seen 60 to 70 percent of scans that come in for a second opinion. There is an ILD protocol by which your scan should be done, so get the scans done that way then you don't have to repeat a scan. Even if the quality is okay then the reporting has to be done well. If only the reporting part is bad, you can send the DVD soft copy to a second CT radiologist for a second opinion. ECHO and Right heart Cath very important for vascular lung diseases. Echo is a good screening test but in Scleroderma where you suspect pulmonary hypertension, Right Heart Cath is required. Immunomodulation and PAH treatments are important. New drugs are being heard of and that is so heartening to note we can slow progression of the lung involvement.

Dr Sujeet Rajan, MBBS, MD - Pulmonary Medicine, DNB - Respiratory Diseases Pulmonologist.
Dr Rajan is a Pulmonologist at Bhatia hospital in Mumbai. He has vast experience of 22 years and specialized in Interstitial lung disease, airway diseases (asthma and COPD), and sleep-disordered breathing. His other areas of practice include TB, especially MDR and XDR-TB.
















