
Vibha Dhoot, 39 from Jaipur shares the journey of her son who was born with major and multiple congenital heart defects and how the family overcame the many challenges, worked through multiple surgeries and complicated treatment protocols to give him a promising future.
Please tell us about your child’s conditions and how and when this was diagnosed. At what age? How did it all start? The early symptoms.
My son was born in 2016 after a full-term pregnancy. He is 9 years old now. All routine sonographies and medical check-ups during pregnancy were normal, and there was no indication of any heart problem before birth. However, immediately after delivery, we noticed that he was blue and struggling. He was taken straight to the NICU even before I could hold him.
I was not informed of any issues after all the regular scans that were done during pregnancy. It was only post pregnancy that I learnt through my doctors and radiologist that these were issues that could have been detected easily through the scans during pregnancy. Knowing this early would have enabled me to be more prepared about my son’s condition and situation.
Subsequent medical tests revealed that he had major and multiple congenital heart defects. Because I had undergone a caesarean section, the full seriousness of his condition was not disclosed to me right away. It took about 11 days before I fully understood the gravity of his diagnosis. Those initial days were extremely critical — doctors kept telling us that the first 24 hours were crucial, then the next 72 hours, then the first week. His oxygen saturation levels remained consistently below 70, and every passing hour felt uncertain.
We were informed that he would need open-heart surgery, but it could not be performed until he was older and stronger. Until then, we were advised to be extremely cautious, as even excessive crying could put stress on his heart. In that sense, his condition was diagnosed immediately at birth, but the journey of understanding, acceptance, and treatment unfolded gradually — and continues even today.
Further investigations later confirmed that my son was also diagnosed with DiGeorge syndrome, also known as 22q11.2 deletion syndrome, a genetic condition caused by the absence of a small portion of chromosome 22. This syndrome can be associated with congenital heart defects, immune system challenges, developmental differences, and other health concerns. In our case, the cardiac involvement was the most significant and immediate challenge.
What were the tests that led to a diagnosis? Was any prenatal screening done? If not, why?
All routine prenatal screenings and investigations were conducted during my pregnancy. There was no known family history of congenital heart disease, and none of the scans showed any abnormalities. Even the detailed anomaly scan performed at around 20 weeks of gestation was completely normal. Since there were no clinical indicators or risk factors, a fetal echocardiogram was not recommended at that time.
After birth, however, when my baby began turning blue and showed signs of breathing difficulty, he was immediately taken for medical observation. This prompted further investigations, including echocardiography (echo) and electrocardiography (ECG), CT scans, which ultimately led to the diagnosis of his congenital heart condition.
This experience highlighted for us how some congenital heart defects may not be detectable during routine prenatal scans and may only become evident after birth, despite appropriate antenatal care.
What was your reaction to the diagnosis? What is the medical prognosis?
My son was diagnosed with a complex form of congenital heart disease — Ventricular Septal Defect (VSD) combined with Pulmonary Atresia and MAPCAs (Major Aortopulmonary Collateral Arteries). The doctors explained that his condition was medically complicated and would require open-heart surgery, including unifocalisation and a Rastelli procedure, to establish proper blood flow between his heart and lungs.
Hearing this diagnosis was devastating. At first, I was completely shattered and found it difficult to even absorb what was being said. The medical terminology, the seriousness of the condition, and the uncertainty of the road ahead felt overwhelming. Like any parent, disbelief came before acceptance.
However, with time, guidance from doctors, and the support of my family, I slowly gathered the strength to face the reality. Accepting the diagnosis did not happen overnight, but once I did, I knew that courage, faith, and resilience would be essential — not just for my child, but for me as a parent walking alongside him through this journey.

What was the initial treatment? And how has the treatment changed over time? How is your child responding to the treatment?
During the first eight months, my son was not on any medication. His condition was managed through very close monitoring and strict preventive care until he was strong enough to undergo surgery.
We regularly monitored his oxygen saturation (SpO₂) levels, as they tended to drop easily. Great care was taken to prevent infections, especially common illnesses such as cold and cough, which could significantly worsen his condition. We were also advised to ensure that he did not cry excessively, as crying would further reduce oxygen levels and place additional strain on his heart and body.
To protect him, we made conscious lifestyle adjustments — social interactions were kept to a minimum, we did not take him outside the house, and visitors were restricted strictly to immediate family members. These precautions, though emotionally difficult, were necessary to keep him stable during those critical early months.
The initial treatment began when my son was eight months old, when he underwent his first open-heart surgery. It was a long and complex procedure that lasted nearly 12 hours, followed by an extended hospital stay of about 20 days. Thankfully, he responded well to the surgery, and an important milestone was achieved — his Ventricular Septal Defect (VSD) was successfully closed.
We were also informed that due to the nature of his condition, a conduit (an artificial connection between the heart and lungs) had been placed during surgery. This conduit does not grow with the body and therefore needs to be replaced every 5–6 years, meaning periodic corrective open-heart surgeries will be a lifelong reality for him.
However, as a postoperative complication, he developed arrhythmia, or an abnormal heart rhythm. For the next year, his heart rhythm was closely monitored. When it became clear that the arrhythmia was persistent, he had to undergo another surgery to have a pacemaker implanted in his abdomen, which he will need for life. The pacemaker will also require replacement at regular intervals.
The need for any change related to the pacemaker is determined through regular monitoring by an electrophysiologist, with follow-up check-ups typically done every six months. During these visits, the pacemaker is thoroughly evaluated to assess battery usage, remaining battery life, and overall device functioning. Based on these reports, doctors can estimate how many more years the battery will last and accordingly plan for a timely replacement, well before it becomes critical.
After a pacemaker change or adjustment, there is generally a short period of observation, but no major stabilization phase is required. From the outside, there are no visible changes in the child’s condition; however, internal changes are reflected clearly in medical reports and device readings.
In terms of daily life, the impact is minimal. My child is able to carry on with routine activities, schooling, and hobbies. Certain precautions are necessary — for instance, protecting the abdominal area where the pacemaker is placed from any direct impact, such as during ball games or rough play. Additionally, we are mindful about avoiding prolonged exposure to strong electromagnetic sources, such as certain airport scanners and keeping mobile devices at a safe distance, as advised by the medical team.
His most recent surgery took place in April 2024, and he continues to respond with remarkable courage to each phase of treatment. Despite the repeated interventions and hospitalisations, his recovery has been steady, and his spirit remains incredibly strong.
What medications is he currently on?
He is not on any type of medication. He just takes Vitamin and calcium supplements.
Have you tried complementary medicine or therapies? If yes, did it help?
We have not tried any complementary or alternative therapies. Given the complexity and seriousness of my child’s heart condition, we chose to rely strictly on evidence-based medical treatment under the guidance of qualified pediatric cardiologists and cardiac surgeons.
I did explore and research complementary options, but I could not find any therapy that was scientifically proven to address his specific condition. For us, it was important not to experiment, but to follow a medically sound path that prioritised safety, accuracy, and long-term outcomes.
What kind of specialists (including Physio/ Occupational therapist/ Psychiatrist etc.) do you consult and how often? Were there any interventions needed other than medication? Why and when was this done?
At this stage, we have not required consultations with additional specialists such as physiotherapists, occupational therapists, or mental health professionals. Fortunately, my child has not shown any need for such interventions so far.
His care has primarily been managed by his pediatric cardiologist and cardiac surgeon, and there have been no requirements beyond medical and surgical treatment. We continue to monitor his physical, emotional, and developmental well-being closely, and if the need arises in the future, we are fully open to seeking additional specialist support.
Do you have a family history of this condition? Was genetic testing done?
There is no known family history of congenital heart disease in our family. This includes both immediate and distant relatives, as far as we are aware. No one in our extended family has experienced a similar condition. Genetic testing was not conducted in our case.
What changes have you made to your and your child’s lifestyle because of this condition?
Living with a congenital heart condition has required us to make certain mindful adjustments to both my child’s and our family’s lifestyle. One of the most important aspects has been focusing on his nutrition. Since his weight and height are below the expected range for his age, I make a conscious effort to ensure that his food intake is balanced, nutrient-dense, and supportive of his overall health and energy needs.
Because his physical activity is somewhat limited, we have adapted by encouraging alternative activities that keep him engaged, happy, and emotionally relaxed. He has developed a strong interest in chess, where he shows remarkable skill, and he is also deeply passionate about music — playing the keyboard and singing bring him immense joy and confidence.
His school life is largely normal and well-balanced. Academically and socially, he participates just like his peers. The only limitations are related to physical sports, as mentioned earlier, and the inability to carry a heavy school bag. For these, the school has been very cooperative and provides the necessary support and accommodations.
His classmates and friends are kind, caring, and naturally protective of him. Even without being fully aware of his medical condition, they look out for him, help him when needed, and include him wholeheartedly in school life. He has lot of friends and he is one of every one’s favourite, students and teachers.
These activities not only help him express himself creatively but also ensure that he remains mentally stimulated and emotionally fulfilled. As a parent, my goal has been to create a lifestyle that nurtures his strengths, protects his health, and allows him to grow with happiness and self-belief despite the challenges of his condition.
He is a single child, and has a wonderful relationship with all his cousins.
How do you navigate work? What kind of accommodations, if any does your employer need to provide?
In the initial years after my son’s birth, I chose to be a full-time caregiver, as his medical needs required constant attention and frequent hospital visits. During that phase, my primary focus was on his health, recovery, and overall well-being.
As his condition stabilised over time, I gradually resumed professional work. Currently, I work from home with flexible hours, which allows me to maintain a healthy balance between my professional responsibilities and my child’s ongoing care. This flexibility has been crucial in ensuring that I am present for his medical needs while continuing to stay engaged in my career. My child has been very supportive and he feels happy seeing me work. I am eternally grateful to him.
How did you mentally/emotionally cope with it all? Pls mention any specific times and issues that were difficult.
Emotionally, the journey has been extremely challenging. There is very little that prepares a parent to see their child on a ventilator or to repeatedly face the uncertainty of major surgeries. Those moments — especially the hours and days before surgery, and the fragile period immediately after — have been the most intimidating and emotionally draining. The fear, helplessness, and waiting can feel unbearable.
Over time, however, I found strength in my child’s resilience. Watching the courage and calm with which he faced each procedure helped me regain my own strength. Children have an extraordinary ability to endure, and his bravery became my anchor.
There was a phase when I constantly questioned, “Why us?” But as my journey continued, I realised that there are millions of children around the world facing their own medical battles, often with far fewer resources. That understanding shifted my perspective from despair to gratitude.
We were fortunate to find the right doctor and the right treatment at the right time, and that has made all the difference. Faith — in God, in medicine, and in the strength of my child — has been central to how I have coped and continue to move forward.
Did you see a counselor for support?
I did not seek formal counselling during this time. Instead, my family and close friends became my strongest source of emotional support. Their presence, understanding, and encouragement helped me navigate the most difficult phases of this journey.
During such times, people often want to help but don’t always know how to ask or what to offer—and that was true in our case as well. My friends and family may not have had the right words, but their presence spoke volumes. Some would simply sit with me in silence, others would check in regularly, listen patiently, or take care of small things without being asked.
There were moments when I couldn’t articulate what I needed, and they sensed it. And ensuring I wasn’t alone during the most difficult days, their quiet, consistent support made all the difference. They didn’t try to fix the situation—they stood by me through it, and that itself was healing. The hospital itself became an unexpected place of connection. Over those long days, I met other parents whose children were fighting similar battles. We shared fears, hopes, prayers, and countless sleepless nights. Slowly, these families became our extended family. Even today, we remain in constant touch, supporting each other through follow-ups, milestones, and setbacks.
Having a reliable support system allowed me to share my fears, draw strength during moments of uncertainty, and feel less alone. While professional counselling can be immensely helpful for many, in my case, the love and support of family and friends played a vital role in helping me cope and stay resilient.
How has your family supported you?
My family’s support has meant everything to me and has been the foundation that held me together through this journey. They stood by me at every step, offering emotional strength, practical help, and constant reassurance during the most difficult times.
In particular, my mother’s support was unwavering. Her strength, patience, and presence kept me going when I felt emotionally exhausted and overwhelmed. There were moments when I would not have been able to move forward without her encouragement and care. This journey would truly not have been possible without my family’s love and support. They formed the foundation that helped me stay strong for my child when he needed me the most.
My husband has been my strongest pillar—standing by me emotionally and financially at every step. Due to the nature of his profession, there were times when we were physically apart, but our unity never wavered. Even from a distance, his constant reassurance, decision-making, and emotional strength gave me the courage to keep going.
During those phases when he could not be physically present, my mother stepped in as my backbone. Her unwavering presence, emotional strength, and silent sacrifices ensured that I was never alone. Together, their support made the impossible feel manageable. This journey would not have been possible without them.
Are you part of any support group? Have support groups been of help? Are you in touch with any global platform connected to this condition?
Yes, I am part of several online support groups related to congenital heart disease and DiGeorge syndrome, primarily through Facebook communities. These groups have been an immense source of support and reassurance. Few are global forums and few are Indian community. I randomly searched and found out about them.
Whenever there is even the slightest doubt — whether related to pre-operative preparation, post-operative recovery, medical concerns, or emotional anxiety — these platforms provide a safe space to ask questions and learn from others who have walked similar paths. Parents and caregivers openly share their experiences, challenges, and coping strategies, which helps reduce fear and brings a sense of calm and clarity.
Being connected to these groups has made me feel less isolated and more informed. Knowing that there is a global community of families facing similar challenges has been both comforting and empowering.
What is your and your child’s present condition? What were some of the challenges you continue to face?
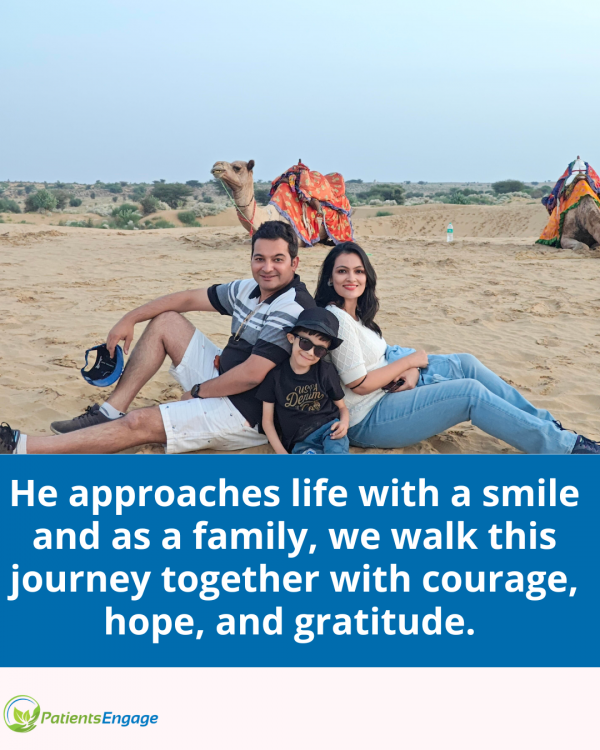
At present, my child is doing well. He is happy, attends school regularly, and actively enjoys his childhood. He is intellectually bright, socially engaged, and curious about the world around him. Seeing him not only participate but excel in everyday activities brings us immense joy and gratitude.
There are, however, ongoing challenges that we continue to navigate. His weight and height remain below average for his age, and at times he feels a little self-conscious when compared to his peers. Due to medical limitations, he is also unable to participate in strenuous physical sports, which can be emotionally difficult for a growing child.
That said, we choose to face these challenges with positivity and acceptance. We focus on his strengths, encourage activities he enjoys, and remind ourselves daily of how far he has come. Despite everything, he approaches life with a smile — and as a family, we walk this journey together with courage, hope, and gratitude. For us, he has always been a warrior.
Have you shared your child’s condition through any social media platform? If so what was the reason to do so?
I have not actively shared my child’s condition on social media in the past. There was no specific reason for not doing so; it was simply a very personal journey, and I chose to process it within my family and close circle.
However, with time, I have grown more emotionally resilient and confident in speaking about our experience. Today, I feel ready to share our story — not for attention, but with the intention of connection and positivity. I believe that when real experiences are shared, they help others feel less alone, offer hope to families facing similar challenges, and create greater awareness and understanding.
If our story can inspire strength, comfort, or reassurance for even one parent or child, then sharing it feels meaningful.
What are some of your learnings that you would like to share for other patients who face similar challenges? What changes would you like to see within the health care system?
One of the most important learnings from this journey is that early awareness, timely medical intervention, and trust in the right healthcare professionals can make an enormous difference. As parents, it is natural to feel overwhelmed and fearful, but staying informed, asking questions, and advocating for your child are crucial. Equally important is accepting that it is okay to take time to process emotions — strength does not mean the absence of fear, but the courage to move forward despite it.
I would also encourage parents to seek support, whether through family, friends, or support groups. Connecting with others who have faced similar challenges can reduce anxiety and provide emotional reassurance. Celebrating small milestones, focusing on the child’s abilities rather than limitations, and maintaining hope play a significant role in sustaining both the child and the family through this journey.
From a healthcare perspective, I believe there is a strong need for greater awareness and early screening for congenital heart disease, including wider access to fetal echocardiography when possible. In addition, more structured emotional and psychological support for parents within hospitals could help families cope better during critical periods. Continued efforts to make specialised cardiac care more accessible and affordable would also ease the burden on many families.
What are you worried about for the future?
Like any parent of a child with a chronic medical condition, my concerns about the future are both practical and emotional. I am aware that my child will need ongoing medical care, including periodic surgeries and medical monitoring, and that uncertainty is something we will continue to live with.
I also worry at times about how he will navigate physical limitations, social situations, and self-confidence as he grows older. As parents, we want our children to feel accepted, capable, and secure in their own skin.
At the same time, I have learned not to let fear define our lives. My focus is on ensuring that he grows up feeling loved, confident, and supported, with access to the best possible medical care. I believe in his strength and in his ability to carve his own path. While the future may hold challenges, it also holds hope — and that is what we choose to hold on to.





