
Pulmonary Physiotherapist Mrinmayee Koltharkar explains what is Oxygen therapy, when it is prescribed, symptoms of low oxygen to watch out for, how it is delivered and types of delivery systems and complications related to oxygen therapy.
Read the second part of the article on oxygen therapy here where she talks of the hygiene protocols, do’s and don’ts and tips on managing travel with oxygen therapy.
Many a times lung patients are prescribed oxygen therapy either after hospitalisations or even during routine doctors visit. They are worried and scared, wondering how long are they going to require it? Are they supposed to be on bed rest henceforth and confine themselves because of it?
Let’s understand all about oxygen therapy.
What is oxygen therapy?
To simply put, Oxygen is in the air we breathe and is necessary to live. When we breathe ‘IN’, oxygen enters the lungs & transfers into the rest of our body via blood. Oxygen fuels our cells to function properly. Our organs use oxygen to do all things & when one doesn’t have enough oxygen in their body, our organs suffer. Over time Hypoxemia (low level of oxygen in the blood) can lead to organ damage and even organ failure.
Some people with lung problem's (and/or sometimes even heart problems) cannot transfer enough oxygen into the blood naturally, that’s when additional (supplemental) oxygen may be needed for their organs to function normally.
How does oxygen therapy help lungs?
Supplemental oxygen does not cure lung disease, but it is an important therapy that improves symptoms and organ function. It proves to be a great medical adjunct to reduce strain on your affected lungs and breathe more efficiently.
Oxygen therapy reduces various symptoms like shortness of breath, reduces fatigue, makes person more active and promotes better sleep & even faster recovery post infections. In short it helps provide better Quality of Life!
What are the symptoms of low oxygen?
Low blood oxygen levels can result in abnormal circulation & one might experience following symptoms,
- Difficulty breathing or shortness of breath (dyspnea)
- Rapid heart rate (tachycardia)
- Chest pain
- Coughing
- Wheezing
- Confusion
- Restlessness
- Dizziness
- Sweating
- Headache
- Bluish color in skin, fingernails and lips (cyanosis)
On what basis is oxygen therapy prescribed?
Your health care provider would perform few diagnostic tests to understand the need for supplemental oxygen.
- Simplest way is by checking room air oxygen saturation by using a pulse oximeter, if it is lower that 88 % at rest or during 6 minute walk test, one would be guided for oxygen therapy at rest or activity accordingly
- Another test is Arterial Blood Gas, in which blood is drawn from an artery & oxygen level in it is tested by machine. If the arterial blood oxygen tension (PaO2) is at/ less than 55 mm of Hg
- If your doctor believes that your oxygen level is dropping exclusively in your sleep ( people with sleep apnea), a nocturnal oximetry is done to check the oxygen saturation levels & prescribed night supplemental oxygen if required
Although the pulse oximeter test is easier, quicker, and less painful than the ABG test, it is not as accurate. Following factors may interfere with the results,
- dirty fingers
- bright lights
- darker skin tones
- nail polish
- poor circulation to the extremities
How do I get an oxygen therapy prescription?
What are the sources of home oxygen delivery?
There are various sources for home oxygen therapy as compared to that used in the hospitals/ clinics. There are two sources and how they are delivered to the patient are the systems. E.g. nasal cannula is used to transport the oxygen to the patient from the source, the cannula can be attached to an oxygen cylinder or concentrator.
Your healthcare provider will help you choose the equipment that works best for you.
1. Oxygen concentrators
Oxygen concentrators provide a safe source of oxygen-enriched air. Oxygen concentrators are devices that draw oxygen from room air & pass it through a series of filters that remove dust, bacteria and other particulates.
A) Stationary (home) concentrators provide an uninterrupted oxygen supply with a flow ranging from 0.5 to 10–15 L/min. They have several ergonomic handles built in, to offer options for lifting or rolling the device. Stationary oxygen concentrators are most commonly used by patients on LTOT (Long Term Oxygen Therapy), as they are cost-effective and are safer than using compressed gas cylinders.

B) Portable oxygen concentrators are the latest technology for LTOT users who desire a small, lightweight and portable oxygen solution in a compact and mobile unit. Portable concentrators vary in weight, size, oxygen flow settings, modes, range and battery life, as well as other specifications. Portable oxygen concentrators though expensive are preferred for ambulatory purpose mainly by people who want to use oxygen outside the home. They provide lesser flow of oxygen as compared to stationary concentrators and thus might not be adequate for all.

For compressed oxygen cylinders, there are various ranges of cylinders available in market, which can be lightweight & portable to even jumbo for home use. A regulator is attached to the cylinder’s top and works like a tap, allowing the safe adjustment of oxygen flow rate provided, in L/min. When the tap is manually opened, the oxygen is delivered to a patient via an oxygen delivery device (e.g. tube with a mask or nasal cannula). A pressure reading (barometer) displays the remaining oxygen pressure in the cylinder, to estimate the amount of oxygen available for supply.

What are the types of Oxygen delivery systems?
1) Low-flow systems provide lower oxygen flow than the actual inspiratory flow (∼30 L/min). Low-flow oxygen delivery systems Include:
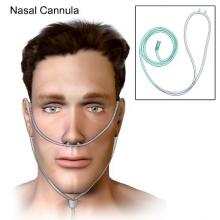
A nasal cannula is the most common oxygen delivery system, used for mild hypoxia. It delivers oxygen into the nasopharyngeal space and can be set to deliver between 1 and 6 L/min. A nasal cannula is convenient as the patient can talk and eat while receiving oxygen, and it is easy to use.
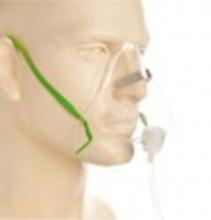
A simple face mask can be set to deliver between 5 and 10 L/min and is indicated when a moderate amount of oxygen is needed. It fits over the patient’s mouth and nose, and has side exhalation ports through which the patient exhales carbon dioxide.
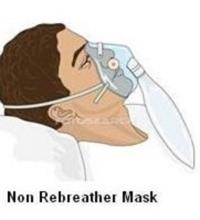
A non-rebreather mask is a low-flow device with high FIO2 . It uses a reservoir bag (∼1000 mL) to deliver a higher concentration of oxygen. A one-way valve between the mask and the reservoir bag prevents the patient from inhaling expired air. It can be set to deliver between 10 and 15 L·min/min.
A) Partial Rebreather (PRB) mask
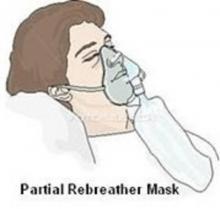
Unlike the non-rebreather mask, there is no oneway valve between the rebreather mask and the reservoir bag and the inspired oxygen and expired air are collected in the reservoir bag.

A Venturi mask is a high-flow device that allows precise measurement of FIO2 delivered. It consists of a bottle of sterile water, corrugated tubing, air/ oxygen ratio nebuliser system, a drainage bag, and a mask.

A high-flow nasal cannula consists of a flow generator, an air-oxygen blender, a humidifier and a nasal cannula.The flow generator can provide gas flow up to 60 L/min
For which conditions is oxygen therapy required?
Here are some common conditions where supplemental oxygen might be required depending on the severity of the condition, either temporarily or long-term,
- Interstitial lung disease (ILD)
- COPD (chronic obstructive pulmonary disease)
- Pulmonary Fibrosis
- COVID
- Pneumonia
- Pulmonary Hypertension
- Acute Respiratory Distress Syndrome (ARDS)
- Lung cancer
- Asthma
- Cystic Fibrosis
- Sleep Apnea
- Certain Heart conditions
- Anaemia
What are the complications of Oxygen therapy?
Oxygen is essential to life, but it has both maximum positive benefit and accompanying toxicity effect. The toxic effects from oxygen therapy can occur based on the condition of the patient and the duration and intensity of the oxygen therapy.
|
Complications |
Precautions |
|
Oxygen-induced hypoventilation/ hypoxic drive |
If patients with a hypoxic drive are given a high concentration of oxygen, their primary urge to breathe is removed and hypoventilation or apnea may occur. It is important to note that not all COPD patients have chronic retention of CO2, and not all patients with CO2 retention have a hypoxic drive. It is not commonly seen in clinical practice. Never deprive any patient of oxygen if it is clinically indicated. It is usually acceptable to administer whatever concentration of oxygen is needed to maintain the SpO2 between 88% and 92% in patients with known chronic CO2 retention verified by an ABG. |
|
Absorption actelectasis |
About 80% of the gas in the alveoli is nitrogen. If high concentrations of oxygen are provided, the nitrogen is displaced. When the oxygen diffuses across the alveolar-capillary membrane into the bloodstream, the nitrogen is no longer present to distend the alveoli (called a nitrogen washout). This reduction in alveolar volume results in a form of collapse called absorption atelectasis. This situation also causes an increase in the physiologic shunt and resulting hypoxemia. |
|
Oxygen toxicity |
Oxygen toxicity, caused by excessive or inappropriate supplemental oxygen, can cause severe damage to the lungs and other organ systems. High concentrations of oxygen, over a long period of time, can increase free radical formation, leading to damaged membranes, proteins, and cell structures in the lungs. It can cause a spectrum of lung injuries ranging from mild tracheobronchitis to diffuse alveolar damage. For this reason, oxygen should be administered so that appropriate target saturation levels are maintained. Supplemental oxygen should be administered cautiously to patients with herbicide poisoning and to patients receiving bleomycin. These agents have the ability to increase the rate of development of oxygen toxicity |
(Table Source: https://opentextbc.ca/clinicalskills/chapter/5-6-complications-of-oxyge…)

Mrinmayee Koltharkar
Pulmonary Physiotherapist |Researcher | International Speaker
CEO & Founder of The Pulmonary Rehab and Caring Conversations
Vice President The Society of CVPR
M.P.Th., B.P.Th., M.I.A.P., Mumbai India | https://linktr.ee/ThePulmonaryRehab
References:
ATS Guidelines for oxygen therapy (https://www.atsjournals.org/doi/epdf/10.1164/rccm.202009-3608ST?role=tab)
BTS Guidelines for administration of oxygen therapy (https://bmjopenrespres.bmj.com/content/bmjresp/4/1/e000170.full.pdf)
American lung association (https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/oxygen-therapy/how-can-oxygen-help-me)
National Jewish Health (https://www.nationaljewish.org/conditions/medications/on-the-go-with-oxygen)
NHS (https://www.nhs.uk/conditions/home-oxygen-treatment/)
















