Bowel (fecal) and bladder (urinary) incontinence is a relatively common side-effect that can occur during cancer treatment. Due to the stigma and under-recognition attached to this condition, quality of life suffers significantly in persons with cancer. Learn more about managing this condition with Prachi P. Narkhede, a MPT Cardiovascular & Respiratory Physiotherapist at Tata Memorial Hospital.
What is incontinence?
It is loss of control of bladder and bowel causing accidental leakage of body fluids and waste. It can be seen in both bowel and bladder.
Bladder Incontinence also known as urinary incontinence, is an automatic or accidental loss, leaking, or dribbling of urine which is a social or hygienic problem.
Bowel Incontinence: Also known as fecal incontinence, it is an automatic/accidental stool or gas leakage which is a social or hygienic problem.
How common is bladder and bowel incontinence in cancer patients?
Bowel and bladder incontinence is very common in few types of cancers like prostate, colorectal and gynecological cancers (cervix, ovarian etc.) It mainly occurs due to the disease itself, cancer related treatments and post-surgical complications.
What are the challenges specifically faced by patients in India?
There are many challenges specifically faced by persons with cancer n India. Some of them are:
- Attitude towards problem and seeking help for the same: many of the people don’t consider urinary incontinence as a health issue and is neglected. Few people still believe it is bound to happen and there is no remedy for it. Shyness prevents them to seek help from the professionals.
- Individual support system: support and coordination from family members is one of the challenges faced by many, especially for women which prevents them from seeking medical attention.
- Priorities and lack of time: people give importance to jobs, household work etc. which prevents them from coming to health care set-ups only for the treatment of a symptom like incontinence.
- Lack of privacy: For people living in small houses, it becomes difficult to perform exercises regularly due to lack of privacy. People get conscious and shy due to presence of other family members which hinders exercising.
- Social taboo and personal beliefs: people are scared to seek medical attention for incontinence thinking of what will their family members and society will think of them. People lack the knowledge about the condition and importance of treatment for the same.
How does incontinence disrupt quality of life?
Incontinence significantly affects a person’s personal, family and social life for both men and women. It is hard for one to accept incontinence as it has a negative effect on their sexuality and privacy. People get embarrassed, do not seek medical attention and this further worsens their quality of life. Discomfort due to feeling “dirty”, “wet”, “smelly”, leads to restriction of social outings/gatherings and day to day activities like shopping, exercises, visiting friends/worship places etc.
People suffering from incontinence experience low physical attractiveness, low self-esteem, body negativity, a reduction of sexual desire, inadequacy and stigmatisation, which can lead to self-isolation, loneliness and depression. Frequent need to use the bathroom affects the basic day to day routine too.
When and why do patients get referred to the Physiotherapy department?
Individuals with anal or bladder cancer, gynaecological cancers (endometrial, ovarian, cervical, valvar and vaginal) and prostate cancer can all experience incontinence due to disease or cancer related treatment. These treatments can directly have an effect on the pelvic region especially pelvic floor muscles. This leads to hardening of the pelvic floor in both males and females with shortening and narrowing of the vaginal canal in females and enlarged prostate, hypermobile urethra in males which leads to incontinence. The patient is referred by their Oncologist to the physiotherapy department when one is planning to undergo cancer related treatments or if he/she has experienced episodes of accidental leakages during their cancer journey. Physiotherapy is administered early on at the onset of symptoms and if incontinence continues to be of moderate severity.
How can care providers (family members) help? What guidance do you provide them?
A Physiotherapist educates the care provider with all the dos and don’ts for the person with cancer. Therapist instructs the care giver on how to take proper care of the suffering person such as:
- Skin care: a caregiver should help the person to practice good skin care after the use of the bathroom. Use of warm water and patting the area dry.
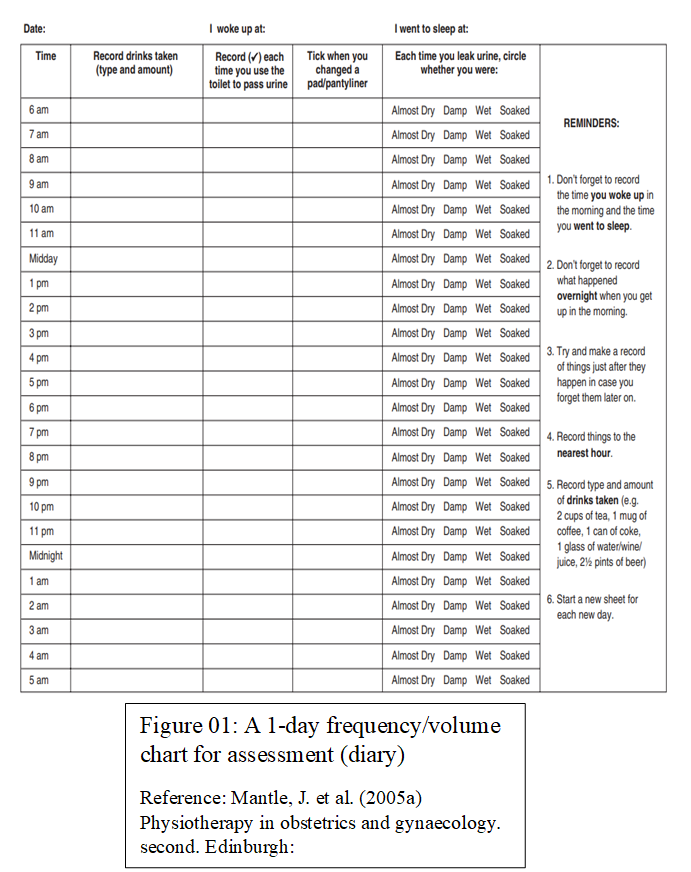
- Maintain diary: a caregiver should help the person to maintain a diary (see figure 1 below) that records the fluid and food intake that can affect the frequency bathroom use.
- Plan: a caregiver should help the person to maintain a bowel and bladder plan (record of the amount of fluid and food intake along with a schedule of the time and frequency to use the toilets)
- Encouragement: a care giver should encourage the person to use bathroom at consistent times (for example- after meals) and also should encourage regular practice of physiotherapy exercises.
Bladder Incontinence
Common presentations in men and women
Urinary incontinence is more common in women than in men. Both men and women can describe urinary incontinence as:
- Experiencing a sense of urgency or unable to “hold urine”.
- Accidental leakage of urine that can dampen the clothes or can be severe enough to saturate clothes.
- Frequent need to urinate.
- Discomfort and pain while urination.
What are causes of bladder incontinence in persons with cancer?
There are many causes of bladder incontinence in person with cancer. These can include:
- Weakness in muscles which control the bladder i.e. pelvic floor muscles.
- Radiation to the pelvis, genital area and abdomen. Various types of chemotherapy or targeted therapy can also lead to incontinence.
- Urinary tract infection.
- Added pressure due to tumor in spine or near bladder.
- Nervous system disorders.
- Gastrointestinal tract obstruction (in the bowel or intestine that may also affect the bladder).
- Bladder irritants like caffeine, alcohol or tobacco.
Why is it more common in women than men? What is the role of estrogen?
The main reasons that lead to urinary incontinence more in women than in men are:
- Weak pelvic floor muscles which are important to support bladder, uterus and urethra.
- Woman’s urethra is shorter than the male urethra and hence the chances of weakness, infection or damage of urethra in females is more.
- Life events like pregnancy, childbirth, menopause and reproductive organ surgeries.
Estrogen helps in regulating the function and growth of vascular and non-vascular smooth muscles of vagina, and it affects the vaginal wall muscles tone and its perfusion. It also regulates the bladder smooth muscle contractility, nerve density and overall structure. Hence estrogen plays a vital role in preventing urinary incontinence.
Post menopause (natural/ due to surgical procedure) estrogen levels are reduced which causes weakness in pelvic floor muscles reduce bladder support and ability to hold the urine. In turn this can cause overactive bladder which can lead to urinary incontinence
How is urinary incontinence diagnosed and measured?
Detailed past and present gynecological history and any history of urine leakage has to be obtained from the person. The current quality of life and activities of daily living has to be assessed.
Physiotherapist use various test to measure and diagnose urinary incontinence. These include the Pelvic floor muscle strengthening by using modified oxford grading system, palpation of the pelvic floor muscles per vagina in female and per rectum in male, 24hours to 48 hours pad test, and urinary (voiding diary).
PERFECT is the mnemonic used for assessment:
P: Power of the muscles, use the Modified Oxford Grading Scale
E -Endurance, the time (in seconds) that a maximum contraction can be sustained
R -Repetition, the number of repetitions of a maximum voluntary contraction
F - Fast contractions, the number of fast (one second) maximum contractions
ECT - Every Contraction Timed, reminds the therapist to continually overload the muscle activity for strengthening.
How can a patient manage urinary incontinence?
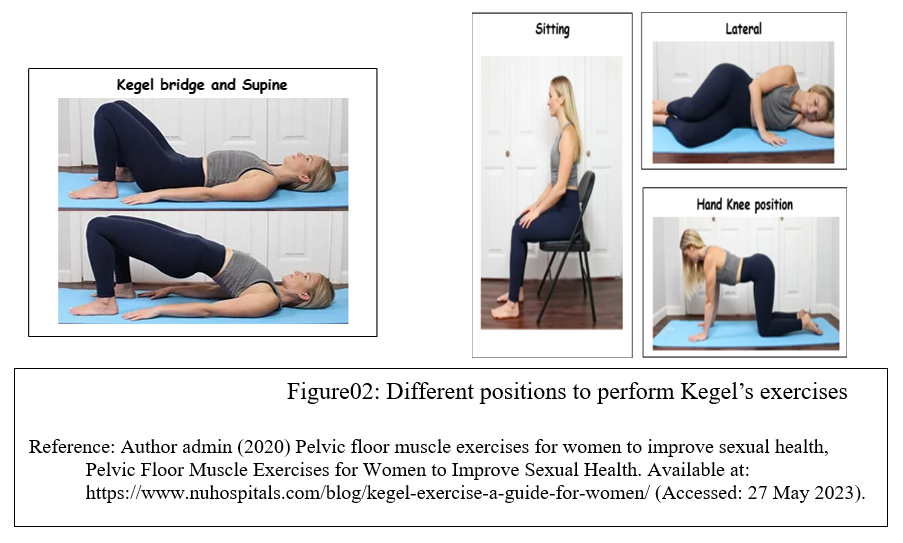
Exercises: Kegel’s exercise is one of the most important part of rehabilitation. Person should perform it appropriately and regularly to gain maximum benefits. Initially a two week trial is given. The person is asked to tighten the sphincter which reflexively inhibits the bladder from having a bladder contraction. One should be persistent as improvement may take up to 4-8 weeks. Initially 5 seconds hold for each contraction and 10 repetitions. Gradually person is asked to increase the time of hold (in seconds) of contractions.
Behavioral therapy:
Behavioral therapy: Physiotherapist can teach a person relaxation technique which helps in controlling urinary incontinence. Person should find some distractions; it will help them to divert there focus from incontinence. A person should have a knowledge about what and how much food to eat to prevent/control urinary incontinence.
Biofeedback:
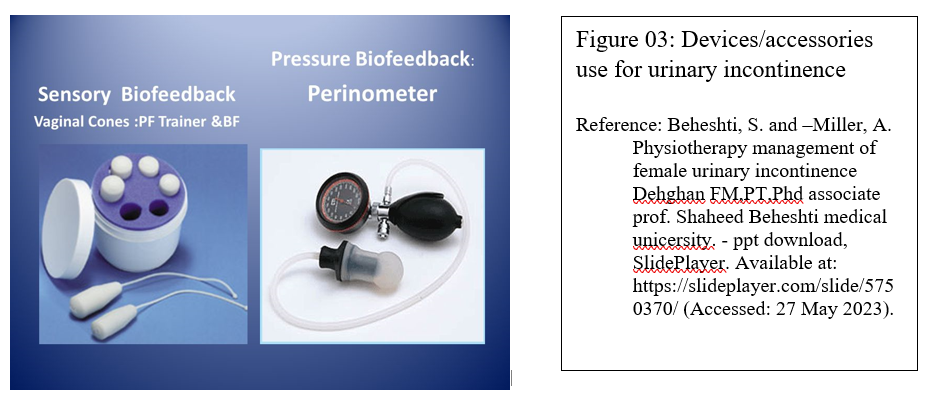
Biofeedback and muscle conditioning, known as bladder training, can alter the bladder's schedule for storing and emptying urine. These techniques are effective for urge and overflow incontinence.1,2 It is used with pelvic muscle exercises and electrical stimulation to relieve incontinence.
a. Do you recommend any product or accessory use?
Yes, Physiotherapists recommend various products and accessory to use in condition like urinary incontinence. Few of them are listed below: -
Perineometer: Used to measure pressure within the vagina and to motivate women to practice pelvic floor exercises. A compressible air-filled rubber portion is inserted in vagina by the women and attached to rubber tubing to manometer, the person is asked to contract the pelvic muscles and note the highest reading on the dial and time of contraction.
Vaginal Cones: In rehabilitation of muscle, resistance in form of weight has been used to increase strength and endurance. This consist of series of five to nine small, progressively weighted cylinders ranging from 10 g to 100 g.
Treatment sessions: insert cones twice a day and walk for 15 mins. Once the cone is retained for 15 min without slip then progress is made to the next cone. Course of 1 month is recommended.
Other accessories like external condom catheters(often a good option for men), diapers, foley’s catheter and tampons are also useful.
b. Daily living:
Avoid heavy lifting, prevention of constipation, weight gain and control obesity if present. Smoking cessation is important if you are a smoker along with maintenance of a fluid and food intake diary.
c. Hygiene:
Keep the area dry and clean, empty your bladder every 2-3 hours when awake and before going to bed. Avoid hygiene products that may irritate you such as perfumed soaps, scented lotions, powder, toilet wipes with alcohol etc.
d. Mental health:
Person with cancer can experience anger, fear, anxiety and reduced sexual drive due to the conditions. Proper counselling of both the person suffering from incontinence and care giver must be done. The caregiver and spouse should provide support to the person with cancer.
Bowel Incontinence
What are the common sign and symptoms of bowel incontinence?
Few of the signs and symptoms of bowel incontinence are unable to control gas or stools, urge to move bowel before it happens and leaking liquid stools or mucus. This is also called as soiling.
What are the causes of bowel incontinence in person with cancer?
Few of the causes for bowel incontinence in cancer patients are weakness of muscle which control bowel movement, constipation, irritable bowel syndrome, diarrhoea, haemorrhoids, rectal prolapse, radiation to the pelvic, abdominal (belly), rectal, or genital area and uncontrolled diabetes.
Are certain people at higher risk?
Yes, people who have uncontrolled diabetes, tumour pressure on spine or near bladder, nervous system disorders like stroke, spinal cord injury, dementia, Parkinson's disease, or multiple sclerosis are at higher risk. In women the most common risk factor is vaginal child birth as it stretches the anal sphincter, vaginal tissues and pelvic floor which can lead to bowel incontinence.
How can patients manage it with Physiotherapy?
Pelvic floor exercises and anal sphincter exercises: These exercises aim to increase the strength of the pelvic floor muscles (mainly levator ani). The anal sphincters are not technically part of the pelvic floor muscle group, but the external anal sphincter is a voluntary, striated muscle which therefore can be strengthened in a similar manner. It helps increase muscle strength and bowel and gas control through tightening and relaxing your pelvic area, anus, and rectum. Electrical stimulation can also be applied to the anal sphincters and pelvic floor muscles to prevent bowel incontinence. Biofeedback: the use of equipment to record or amplify and then feedback activities of the body.
Tips for daily living:
Managing symptoms of pain, flatulence etc: Accumulation of gas in digestive tract leads to pain. Most of the stomach gas is released when the person burp. Eating habits, such as eating too quickly, drinking through a straw, chewing gum, sucking on candies or talking while chewing results in more swallowing of air, so these should be avoided. Carbonated beverages, such as soda and beer, increase stomach gas and person suffering from incontinence should avoid taking them.
Toilet use at home/outside: It is recommended to follow bowel care plan (move your bowels at the same time every day and eating food at same time). must use toilet before going to sleep and after waking up, before the start of the journey if travelling to avoid soiling
Diet: Monitor and journal food and drink daily . Try to eat at same time every day. Seek the help of a dietician if required.
Supplies/Accessories: Your doctor may prescribe moisture-barrier cream for the anal area, wick pads or disposable underwear. Carry extra pair of underwear, faecal deodorants.
Travel tips: A person should monitor the food intake before and during their travel to prevent the urge to use the toilet 1,2 Consider emptying the bowel before travelling.

Prachi P. Narkhede, a MPT Cardiovascular & Respiratory Physiotherapist at Tata Memorial Hospital
References:
- Mantle, J. et al. (2005a) Physiotherapy in obstetrics and gynaecology. second. Edinburg.
- Michael. D Stubblefield et al. (2009) Cancer Rehabilitation, Principals and practice first edition.
- Mishra, GDaxa & Dinesh, Kumar & Pathak, GAjay & Vaishnav, Smruti. (2020). Challenges encountered in community-based physiotherapy interventions for urinary incontinence among women in rural areas of Anand District of Gujarat, India. Indian Journal of Public Health. 64. 17. 10.4103/ijph.IJPH_436_18.
- Corrado B, Giardulli B, Polito F, Aprea S, Lanzano M, Dodaro C. The Impact of Urinary Incontinence on Quality of Life: A Cross-Sectional Study in the Metropolitan City of Naples. Geriatrics (Basel). 2020 Nov 20;5(4):96. doi: 10.3390/geriatrics5040096. PMID: 33233663; PMCID: PMC7709681.
- Bladder and bowel incontinence (no date) Urinary Incontinence. Available at: https://www.cancer.org/cancer/managing-cancer/side-effects/stool-or-uri… (Accessed: 25 May 2023).
- Tzur T, Yohai D, Weintraub AY. The role of local estrogen therapy in the management of pelvic floor disorders. Climacteric. 2016 Apr;19(2):162-71. doi: 10.3109/13697137.2015.1132199. Epub 2016 Feb 2. PMID: 26830033.
- Nahon I. Physiotherapy management of incontinence in men. J Physiother. 2021 Apr;67(2):87-94. doi: 10.1016/j.jphys.2021.02.010. Epub 2021 Mar 19. PMID: 33753017.
- Author admin (2020) Pelvic floor muscle exercises for women to improve sexual health, Pelvic Floor Muscle Exercises for Women to Improve Sexual Health. Available at: https://www.nuhospitals.com/blog/kegel-exercise-a-guide-for-women/ (Accessed: 27 May 2023).
- Beheshti, S. and –Miller, A. Physiotherapy management of female urinary incontinence Dehghan FM,PT,Phd associate prof. Shaheed Beheshti medical unicersity. - ppt download, SlidePlayer. Available at: https://slideplayer.com/slide/5750370/ (Accessed: 27 May 2023).