People with diabetes are at a higher risk of high blood pressure. High Blood pressure also increases the risk of diabetes. This co-existence leads to cardiovascular conditions, stroke, kidney disease, visual impairment and more. Read more to understand how you can manage both these conditions to improve your health outcomes.
The International Diabetes Federation estimated that 72.9 million adults in India had diabetes in 2017, and this number would grow to 134 million by the year 2045. Studies show that people with diabetes are twice as likely to get hypertension compared to the non-diabetic population. Hypertension by itself is known to increase the risk of developing both micro and macrovascular diseases. With diabetes added to the mix, the impact is greater on both the cardiac and vascular systems. A US study from 2012 found that 50-80% of people with Type 2 and 30% of people with Type 1 diabetes have high blood pressure. In type 2 diabetes patients, hypertension is associated with hyperinsulinemia and insulin resistance. In India, the increase in the co-existences of diabetes and hypertension has been described as a dual epidemic.
How does diabetes cause hypertension?
We know that a person with diabetes is unable to process glucose in their body due to lack or low insulin production or insulin resistance. Insulin is the hormone made by the pancreas that helps to process the glucose from food into energy for our cells. In persons with diabetes, the glucose is not processed and as a result accumulates in the body. It enters the bloodstream and collects in the blood vessels and kidneys causing the blood vessels to lose their ability to stretch and become stiff, thereby causing the pressure in the blood to rise. If there has been similar damage to the kidneys, there is fluid accumulation in the body as well. Insulin resistance, where the body is unable to use the body insulin effectively thereby causing increase in the blood sugar levels and to a higher risk of hypertension.
How are hypertension and diabetes interlinked?
Hypertension is now known as an emerging risk factor for diabetes. Several studies in 2015 were meta-analysed and published in the Journal of the American College of Cardiology (JACC) to find that people with normal blood pressure had low to no risk of diabetes but as the blood pressure increased so did the risk of diabetes. This causal effect may be due to inflammation of tissue cells over time.
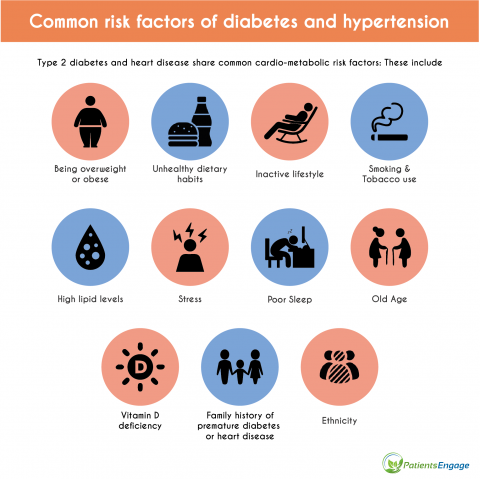
What are the risk factors?
Type 2 diabetes is known to be a risk factor for hypertension and vice-versa. Additionally, since they are both components of the Metabolic Syndrome, hypertension and diabetes share several common risk factors. These include.
- Being overweight or obese
- Unhealthy dietary habits
- Inactive lifestyle
- Smoking & Tobacco use
- High lipid levels
- Stress
- Poor sleep
- Old age
- Ethnicity
- Vitamin D deficiency
- Family history of hypertension and/or diabetes
Why is it important to control both sugar and blood pressure levels?
Control of the key factors in both the conditions viz glucose and blood pressure levels in the body are essential in preventing further complications from the existing co-morbidities. Some of these complications include:
- Further damage to the blood vessels leading to Coronary Heart Disease, Heart failure etc.
- Transient ischaemic attack, Stroke.
- Poor functioning of the kidneys causing fluid retention and kidney diseases.
- Peripheral vascular diseases in the limbs due to atherosclerosis & poor circulation.
- Gradual impairment of blood vessels in eyes causing retinopathy
How to control diabetes and hypertension?
If you have either Diabetes or Hypertension, keep a close eye on your blood glucose and blood pressure levels by following the screen, monitor, treat and manage protocols mentioned below.
1. Screen
Screening is evaluation of a person’s current health and any risk factors for further complications. Screening tests will be prescribed by your doctor every 3 to 6 months depending on your risk factors. During your doctor’s appointment, your blood pressure levels will be checked at the clinic. If a patient is found to have higher than usual blood pressure, the measurement should be repeated on another day. Some patients may be sent home with a 24-hour Holter monitoring device.
Glucose levels are checked via blood tests. Before going in for your check-up, your doctor will prescribe a few of the tests to be done beforehand. These include fasting, 2-hour post-meal, random and haemoglobin A1c test. Levels will be matched to your previous test results along with your daily log to check for any fluctuations. If indeed, there are any changes, the doctor will assess all possible triggering factors and may recommend medication and/or lifestyle adjustments.
2. Monitor
Monitoring is routine evaluation of your blood glucose and blood pressure levels. Patients are recommended to purchase a glucometer and BP machine and take readings at home. This is the most effective way to know your baseline levels and keep track of them in daily life.
3. Treat
Correcting your blood glucose levels and keeping the HbA1c levels below 7% is the goal of all diabetes drugs. Along with your diabetic medications, the goal of your hypertensive drugs should be to maintain a blood pressure of less than 140/90mmHg. ACE inhibitors, dihydropyridine CCBs, ARBs, and thiazide-like diuretics have shown to be the preferred drug for blood pressure control with improved clinical outcomes.
This is important to assess because all the drugs taken by a patient should not counter-interact with each other. We now know that certain diabetic medications affect fluid and blood pressure levels directly. For example, Sodium-glucose cotransport 2 inhibitors and Glucagon-like peptide 1 inhibitors are associated with causing reduction in both systolic and diastolic blood pressure. On the other hand, insulin can further promote salt and fluid retention in the body worsening hypertension. Hence close monitoring and screening will help in providing the patient with the best pharmaceutical treatment. Over-the counter medications like NSAIDs and aspirin can affect blood pressure levels too. Herbal and homeopathic medicines should only be taken with the consent of the treating doctor as they contain hidden sugars and other elements.
4. Manage
Along with medicines, modifications in daily routine of the patient are equally important if diabetes and hypertension are to be controlled. Approach to changes in life should be viewed as long-term changes in daily living. Only if it’s a behavioural change, will it aid in sustained long-term maintenance of the chronic disease. Note that recommended diet and life patterns should be adapted to suit the patients and their families keeping social, financial, and cultural differences in mind. Lifestyle changes should incorporate the following:
- Cessation of all tobacco products
- Limiting alcohol intake to less than 4-5 units per week.
- Change in eating habits
- Reducing salt intake and increasing potassium intake
- Cutting down on sugar in foods and beverages
- Consuming more fruits and vegetables
- Avoiding processed, preserved, and cured foods
- Limiting intake of fried and fatty food products
- Increasing physical activity including some form of daily exercise
- Decreasing sedentary time
- Losing excessive body weight
- Practicing ways to reduce stress
Conclusion
Chronic hyperglycemia (high glucose levels) and hypertension (high blood pressure levels) are associated with long-term damage and dysfunction of various systems in our body. The best way to prevent your chances of getting diabetes or hypertension are to assess and reduce all your modifiable risk factors. If you have any of the mentioned risk factors, make sure to speak to your doctor and discuss how to keep your levels under control.
Early detection can reduce the burden of one or both these chronic conditions. Patients who have either of the conditions are recommended to screen regularly, monitor often, get the right treatment, and make the smart lifestyle alterations to lead a healthy and long life.
Issued as part of the public education series by Boehringer Ingelheim India and PatientsEngage
References:
- Kim MJ, Lim NK, Choi SJ, Park HY. Hypertension is an independent risk factor for type 2 diabetes: the Korean genome and epidemiology study. Hypertens Res. 2015;38(11):783-789. doi:10.1038/hr.2015.72
- Ian H. de Boer, Sripal Bangalore, Athanase Benetos, Andrew M. Davis, Erin D. Michos, Paul Muntner, Peter Rossing, Sophia Zoungas, George Bakris. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care Sep 2017, 40 (9) 1273-1284; doi: 10.2337/dci17-0026
- American Diabetes Association. Screening for Diabetes. Diabetes Care Jan 2002, 25 (suppl 1) s21-s24; doi: 10.2337/diacare.25.2007.S21
- What to Know About Diabetes Prevalence in India. https://www.healthline.com/health/diabetes/diabetes-in-india










