
Crohn’s Disease, IBD, IBS are sometimes used interchangeably. We break down Crohn’s disease, how it is different from these other conditions and explain the symptoms, causes, treatment and management of Crohn’s Disease.
Overview of Crohn’s Disease
To begin with, let’s understand that irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are two different gastrointestinal disorders, as the terms sound similar and may have some overlapping symptoms, it may use them interchangeably and they can be confusing.
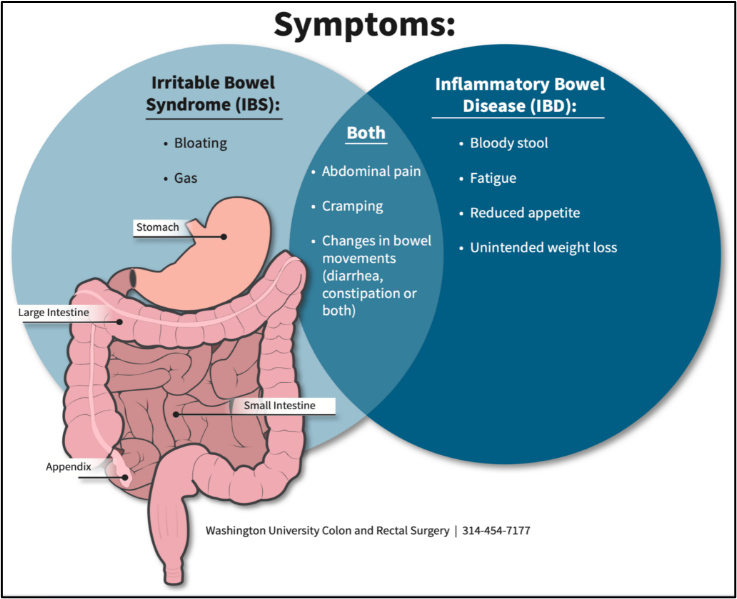
Irritable Bowel Syndrome (IBS)
It is classified as a syndrome (group of symptoms) and does not cause any inflammation.
There is no abnormality detected in the colon during examination and it does not pose a threat to hospitalization and or surgery.
There is no increased risk for colon cancer.
To know more about IBS visit: https://www.patientsengage.com/conditions/irritable-bowel-syndrome/types-stages
Inflammatory Bowel Disease (IBD)
It is classified as a disease and usually causes destruction of the wall of the intestine with inflammation. There are 2 types of conditions with overlapping symptoms that come under IBD, namely Crohn’s disease and Ulcerative colitis. The diagnosis is confirmed on biopsy combined with imaging and blood tests.
Crohn’s Disease
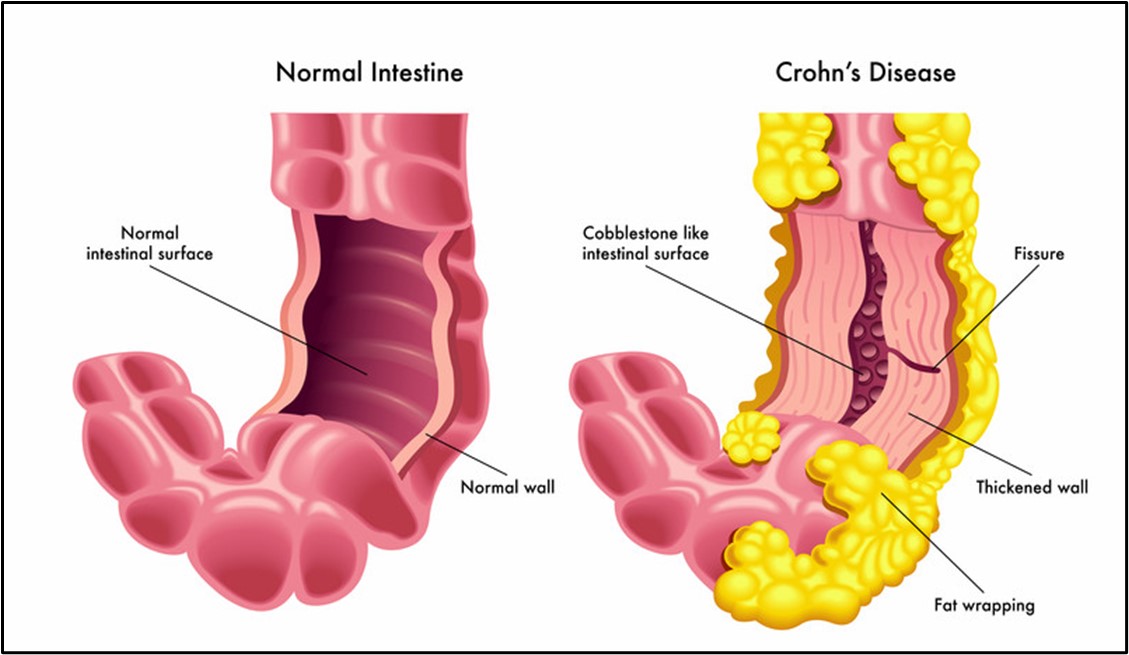
It is a part of the spectrum of the inflammatory bowel disease in which inflammation causes injury and breakdown of the wall of the intestines.
The usual pattern is patchy, causing lesions with gaps referred to as "skip lesions."
It is a prolonged (chronic) condition.
It usually begins between the ages of 15 and 40.
Possible Causes and Risk factors of Crohn’s Disease:
The exact cause is still unknown.
Sometimes, a viral or bacterial infection may activate the immune system in the intestine, and it continues to stay active, thus causing inflammation even after the infection subsides.
Specific genes passed on from the parents may increase the risk of developing Crohn's disease, with the right triggers like an infection.
Symptoms during a “Flare Up”
- Mid or lower abdominal pain that worsens after meals
- Loose stools that may have blood in it
- Perianal sores
- Discharge of pus/mucus from the anal area
- Painful bowel movements
- Mouth sores/ulcers
- Loss of appetite
- Fleeting joint pains or back pain
- Pain and or changes in vision
- Weight loss with usual dietary intake
- Fever
- Generalized weakness or fatigue
- Stunting of growth and or delayed puberty in children.
To read about the personal experience of a patient with Crohn’s please visit: https://www.patientsengage.com/personal-voices/learning-live-flares-ebbs-crohns-disease
Tests for Diagnosing Crohn’s Disease
Blood tests.
They usually reveal signs of inflammation like a high white blood cell count.
Crohn's disease may interfere with the absorption of vitamin B12, that can cause anemia (low hemoglobin), reduced red blood cells count and deficiency of vitamin B12.
Autoantibody tests.
Abnormal antibodies may be detected in the blood of people with Crohn's disease.
Stool tests.
Used to detect infections that may be a possible cause of symptoms.
Upper gastrointestinal (GI) Barium X-rays.
X-ray taken after consumption of a barium solution. It may detect narrowing of the small intestine, ulcers, or fistulas. These abnormalities are detected more often in Crohn's disease than in ulcerative colitis.
Flexible sigmoidoscopy or colonoscopy.
A tube with a camera is inserted into the rectum, which allows visualization of the large intestine and is also used to get a biopsy (sample) from there.
Biopsy.
During colonoscopy or sigmoidoscopy, the doctor takes a small sample of tissue from the wall of the intestine, which is then for signs of inflammation and is used to get a confirmed diagnosis of Crohn's disease.
MRI.
It is used to visualize the areas of Crohn's disease involvement.
Wireless capsule endoscopy.
This test requires the patient to swallow a pill- video camera to help visualize the live pictures of the small intestine wirelessly.
Treatment of Crohn’s Disease
Medications:
- To prevent the inflammation of the intestines, for mild disease, steroids and/or anti-inflammatory drugs called amino-salicylates (similar to Aspirin) are prescribed by the doctors.
- Antibiotics to prevent and treat infections.
- Anti-diarrheal medication to control diarrhea
- Immunomodulators to reduce and suppress inflammation.
- The newest drugs approved for treatment of Crohn's disease are tumor necrosis factor (TNF) inhibitors and other injectable treatments.
Surgery:
Usually done for bowel obstruction, fistula, etc.
Management of Crohn’s Disease
Since Crohn’s is a lifelong condition and has a waxing and waning course, the management involves mitigation of symptoms and associated food intolerance and nutritional deficiencies.
- Nutritional deficiencies:
Vitamin B12 deficiency is common in patients with Crohn's disease or intestinal surgeries.
Iron deficiency is also known to occur in patients with Crohn's disease.
Folate deficiency may be seen due to poor dietary intake or due to some medications used for treatment, like sulfasalazine, that may interrupt the folate metabolism.
Occasionally, Crogns may cause anemia that is unresponsive to replacement therapy(refractory anemia), it is managed by using synthetic erythropoietin. - Protein calorie malnutrition:
In cases of severe colitis, there may be low protein and albumin levels in blood that are also indicators of severity and may require hospitalization and intravenous parenteral nutrition.
Patients with chronic severe malnutrition with massive resection of parts of the small intestine may need to be on home intravenous hyperalimentation therapy. - Low-fibre diet:
Low-fibre diet may help when the symptoms are active.
Prevention of Crohn's Disease:
- Prevention of symptoms: Knowing the family history and seeking early medical attention in case of changes in bowel habits like abdominal pain, diarrhea, weight loss or frequent vomiting may be helpful in early diagnosis and treatment and therefore preventing complications and severity.
- Regular heath checks may help in keeping the gut healthy and maintaining optimal gastrointestinal tract health.
- Dietary changes: Consuming a nutritious and -balanced diet low in fiber may be helpful in reducing any irritation to the inflamed intestinal wall of the intestines. Increase consumption of food that improves gut health, like apples, pureed vegetables, and bananas.
- Regular exercise and de-stressing: Regular exercise and meditation help to maintain optimal health and also reduce stress, which is a trigger for Crohn’s disease.
REFERENCES:
- Crohn's & colitis foundation. “IBS vs IBD | Crohn’s & Colitis Foundation.” Crohn’s & Colitis Foundation, 2019, www.crohnscolitisfoundation.org/what-is-ibd/ibs-vs-ibd.
- “Inflammatory Bowel Disease or Irritable Bowel Syndrome? | Department of Surgery | Washington University in St. Louis.” Surgery.wustl.edu, surgery.wustl.edu/inflammatory-bowel-disease-or-irritable-bowel-syndrome/.
- “Diet and Nutrition.” Crohn’s & Colitis Foundation, www.crohnscolitisfoundation.org/diet-and-nutrition?trackBlock=true&bloc….
- Harvard Health Publishing. “Crohn’s Disease - Harvard Health.” Harvard Health, Harvard Health, 15 Nov. 2018, www.health.harvard.edu/a_to_z/crohns-disease-a-to-z.
- Botoman, V. Alin, et al. “Management of Inflammatory Bowel Disease.” American Family Physician, vol. 57, no. 1, 1 Jan. 1998, pp. 57–68, www.aafp.org/pubs/afp/issues/1998/0101/p57.html.
- “Inflammatory Bowel Disease Treatment & Management: Approach Considerations, Symptomatic Therapy/Supportive Care, Overview of Therapy.” EMedicine, 14 June 2021, emedicine.medscape.com/article/179037-treatment?form=fpf&scode=msp&st=fpf&socialSite=google&icd=login_success_gg_match_fpf&isSocialFTC=true#d21. Accessed 12 Dec. 2023.
- colon90210. “Prevention of Crohn’s Disease.” Los Angeles IBD, IBS, and Colon Cancer Surgeons, 5 Nov. 2013, colon90210.com/crohns-disease/prevention-of-crohns-disease. Accessed 29 Dec. 2023.
















