We have all struggled with a change in consistency of stools whether it’s diarrhoea or constipation or something in between. We have also at some point seen a change in colour or texture of the stools of our kids or ourselves and wondered what that could mean. We are here to tell you everything a change in your stools could mean and when a stool test is needed.
Stools or faeces are solid waste products that are formed in the large intestine and is made up of undigested food waste after the nutrients have been absorbed. Stool is made up of 75% water and 25% solids (mostly microbes, fibre and other waste). As the food moves through the intestine the water gets reabsorbed and the waste is compacted to gain some consistency and shape that can be excreted.
One should know that both change in frequency and consistency of the stools may indicate a possible need for change in diet and lifestyle and or a possible infection/pathology.
Related Reading: What does the colour of your urine mean?
It is a well-established fact that all chronic issues are related directly to gut health in many ways and thus regular bowel movements and the quality of stools holds value. Let’s talk about what the colour of your stool means.
Colour of Stools:

Normal: Usually shades of brown due to the presence of bile in it (yellow/brown and dark brown) depending on the food consumed.
Gray or clay stools: Usually caused by the absence of bile in the stools. It may be due to an obstruction to the flow of bile from the bile duct to the intestine caused by gall bladder stones, tumour or pancreatic issues. Usually, the colour change will happen gradually over a period of time. You need to see a doctor.
Black stools (No odour or stickiness): Due to medications containing iron or Bismuth.
Black Sticky stools: Usually indicates bleeding from the stomach or upper part of the intestine from a possible ulcer. It may be foul smelling.
Green stools: When the movement of the stools is very swift through the intestines, the bilirubin does not get the chance to undergo chemical change and hence the colour remains green. Sometimes consumption of green vegetables like beetroot or food with green dyes may also impart a green colour. Iron supplements also cause stools to turn a dark green almost blackish colour
Red or Maroon stools: Usually indicates bleeding from the lower part of the intestine like colon or rectum and doesn’t change colour as it doesn’t mix with digestive enzymes. Sometimes consumption of vegetables like beetroot or cranberries may also impart a bright colour. Seek immediate medical attention. Sometimes the bleeding may be due to passage of hard stools due to chronic constipation which causes local issues like piles or fissures.
Yellow stools: Possibly due to undigested fat in stools. Usually caused by pancreatic issues such as obstruction of pancreatic duct, chronic pancreatitis, etc. It may also be caused by Cystic Fibrosis where the stool is yellow and sticky. Some weight loss medications also cause the stools to be yellow and sticky as they limit the absorption of fat by the intestines.
Consistency of Stools:
*Refer to the images for types.
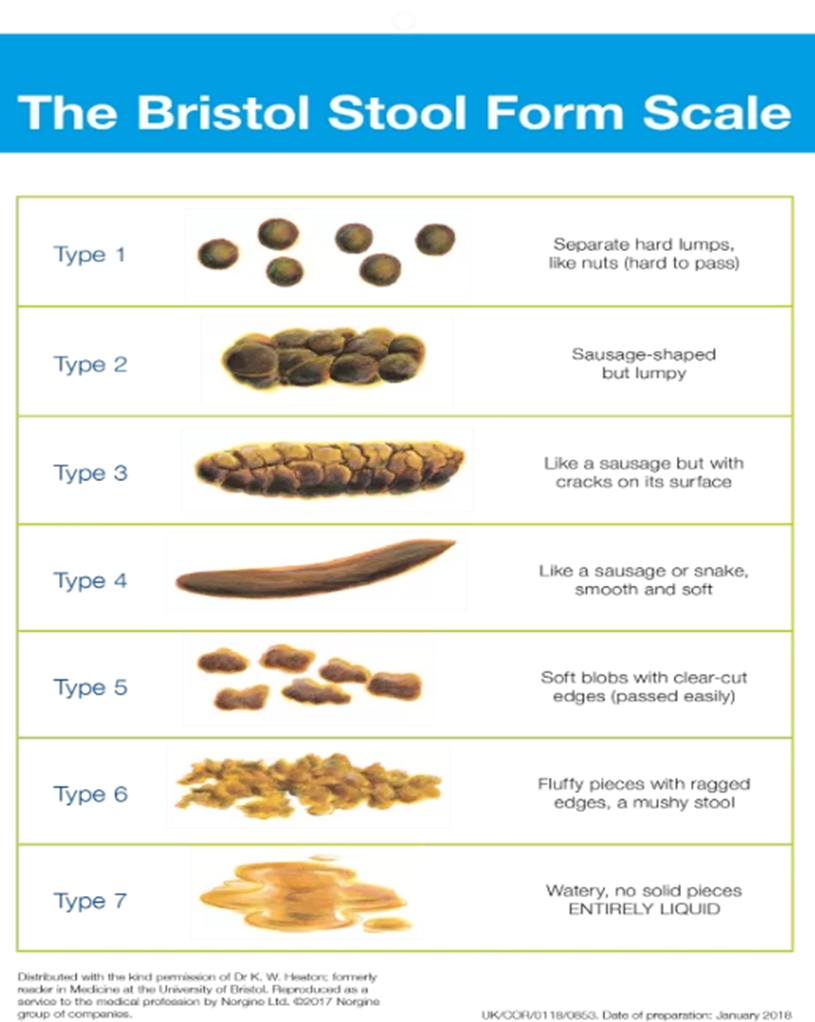
Figure 2: https://www.continence.org.au/bristol-stool-chart
Normal: Stools should be solid and soft and should be passed with ease. Type 3 & 4.
Constipation: Hard and pellet-like. May cause the urge to strain for passing stools and difficulty in passing. See Type 1 & 2.
Diarrheal: Type 5 indicates a lack of fibre and type 6 & 7 suggests an inflammation/infection of the gut. The stools may be watery and projectile when one has food poisoning (gastroenteritis). Sometimes in the initial phases of a viral fever, may have transient loose stools that are watery and usually last a day or two.
Dysentery: Sometimes the stool may be foul smelling with mucus and blood in stools which is indicative of a bacterial or protozoal infection. In this case one should definitely see a doctor as a course of antibiotics as per discretion.
Menstruation and Stools:
Menstruation causes a shift in the bowels due to the hormonal influence. In general, menstrual changes may cause an increase in bowel movements.
Diarrhoea: Increase in prostaglandins hormone that causes shedding the uterine wall during a period, can also cause a similar effect in the gut and also cause an increase in contraction of the rectal muscles that may cause diarrhoea.
Constipation: Progesterone hormone that thickens the uterus during the menstrual cycle may cause constipation around and a few days after ovulation.
Frequency of stools:
The interim period between each bowel movement is variable person to person. Generally, it should not be longer than 3 days before one passes a stool.
Constipation means when a person has infrequent stools or difficulty in passing stools. It means when a person has passed stools hard, dry stools for <3 days a week.
Diarrhoea is defined as passage of 3 or more loose or liquid stools per day. It maybe acute (lasts for 1-2 days), persistent (lasts >2 weeks and <4 weeks) or chronic (lasts >=4 weeks).
Aberrant bowel movements are usually suggestive of poor gut health, and one should seek the advice of a doctor.
Chronic diarrhoea with abdominal pain and or indigestion and bloating may indicate IBD (Crohn’s disease and Ulcerative colitis) and should be addressed with a doctor.
Sometimes a flare up of IBD could also cause constipation which may alternate with diarrhoea.
Control Over Bowel Movements:
One should be able to able to hold the urge to pass stools. Inability to do so may be due to anatomical or pathological issues that need to be assessed at a doctor office.
Faecal incontinence means the leakage of liquid, solid stools or mucus from the anus. This may be due to diarrhoea, muscle or nerve damage in the area or prolapse of pelvic organs among many other causes.
How to Ensure a Healthy Gut and Bowel Movements
- Drink lots of fluids: Consume at least 8-10 glasses of water or fluids per day. The amount may need adjustment as per the environmental temperature. Hot humid weather may cause loss of water via sweating and therefore more water intake may be needed.
- Regular exercise: Regular physical activity and exercise is known to boost metabolism and bowel movements.
- Consume fibre in diet: Adults should consume 22-34gms of fibre per day. Soluble fibre absorbs water from the food and makes it into a gel which in turn slows down digestion. Fiber is found in nuts, seeds, lentils, beans and some fruits and vegetables. Insoluble fibre adds bulk to the stools and is found in whole grains, wheat bran and vegetables.
- Use the toilet when you feel the urge: One should not ignore the urge to pass stools. Building a routine helps to prevent habitual constipation.
When is a Stool Test Prescribed
- Blood in stools
- Mucus in stools
- Diarrhoea > 3 days
- Loose stools with nausea or vomiting and or fever
- As a part of work up to diagnose IBD or IBS.
- Routine test for food handlers
How to submit a stool sample?
A sterile plastic box is usually provided by the lab. To catch the stools before they hit the water in the pot, one may place a clean disposable container, or a cling film (plastic wrap) over the rim of the toilet. The container should be filled halfway, and the lid should be shut.
For faecal occult blood sample: Stop pain killers like NSAIDs, Aspirin, Vit C , Iron supplements and red meat for a week prior if possible, else at least 48-72 hours before the test.
Avoid taking antacids and any antibiotics 48 hours before a stool sample collection.
Types of Stool Tests:
- Stool Routine Microscopy: Done to rule out parasitic and bacterial infections. It provides information on the following:
- The colour of the stools
- Consistency of stools
- pH of the stool sample
- Hidden occult or blood
- Amount of stools
- Shape of stools
- Odor of stools
- Presence of mucus
- Different types of cells in the stool
- Stool to test for Occult Blood: Detects any blood in stool that tells us about potential bleeding from the gut.
- Stool DNA test for detecting polyps or colon cancer.
What Does Your Stool Test Result Mean?
- High level of fat in the stool: Pancreatitis, celiac disease, cystic fibrosis, or other conditions that affect the absorption of fats.
- Undigested meat fibre: pancreatitis.
- Low pH: Malabsorption of carbohydrate or fat.
- High pH: Possible colitis, cancer, or use of antibiotics.
- Blood in the stool: Bleeding from the gut.
- White blood cells in the stool: Possible inflammation in the intestines due to ulcerative colitis, or a bacterial infection.
What Conditions Are Checked in a Stool test:
- Infections: Bacterial, viral, or parasitic infections, such as Salmonella, Shigella, Campylobacter, Giardia, and C. Difficile.
- Bleeding: Hidden blood in the stool, which could indicate cancer, polyps, haemorrhoids (piles), (IBS)inflammatory bowel disease or IBD (inflammatory bowel disease)
- Issues related to gut health and digestion: Poor nutritional absorption, malabsorption syndrome, colitis, diverticulosis, or exocrine pancreatic insufficiency.
- Anal fissures
- Anaemia
- Stomach ulcers
- Cancer: Colorectal cancer, or precancerous polyps
References:
- “Poop Colour Changes: What Does the Colour of Your Stool Mean?” EMedicineHealth, www.emedicinehealth.com/stool_colour_changes/article_em.htm.
- “Timing Is Everything: Study Finds Link between Bowel Movement Frequency and Overall Health.” ScienceDaily, www.sciencedaily.com/releases/2024/07/240716122711.htm.
- Restivo, Jenette. “8 Ways to Get Constipation Relief.” Harvard Health, 10 Aug. 2023, www.health.harvard.edu/staying-healthy/8-ways-to-get-constipation-relief.
- “Fecal (Bowel) Incontinence: Causes, Tests & Treatment.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/14574-fecal-bowel-incontinence.
- “Stool Analysis.” UK HealthCare, ukhealthcare.uky.edu/digestive-health-program/diagnosis/stool-analysis.
- Cleveland Clinic. “Stool Test.” Cleveland Clinic, 2023, my.clevelandclinic.org/health/diagnostics/25210-stool-test.