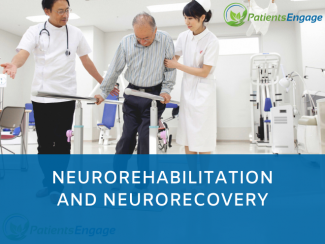
Dr Abhishek Srivastava, Director, Centre for Rehabilitation at Kokilaben Hospital, Mumbai explains the approaches to neurorehabilitation after stroke and how applying the four types of neuroplasticity can help a patient recover and live independently.
Stroke is the leading cause of disability in adults. For Patients, its end of road, for Family its beginning of a burden, for Physicians its interventions, for Organization its investment and for the Nation its loss of Disability Adjusted Life Years. Stroke can affect many parts of the brain causing multiple deficits including, cognitive, behavioral, visual, speech, language, swallow, sensation, movement, muscle tone and sphincter functions.
There are two types of recovery after stroke, first is spontaneous neurological recovery which happens in first 3-6 month primarily due to resolution of local injury and can be modified by newer interventions. The second type is functional recovery and the time period is unlimited!! it’s primarily due to the intensive training triggering newer /alternative electrical circuits in the brain. Similarly, there are two different approaches of neurological rehabilitation, first is compensatory approach, for example, if someone doesn’t have movements in leg causing difficulty in walking and we gave him a stick to walk. Second is remediational approach, in which we try to minimize the impairment or improve power in the leg muscles so a person can walk better and reduce the chances of using a stick to walk. This ability of brain to restore the functional by minimizing the impairment depends upon formation of new / alternative circuits in the brain. This inherent but not widely known ability of the brain to change in response to a triggered stimulus is called as neuroplasticity.
Neuroplasticity, capacity of neurons and neural networks in the brain to change their connections and behaviour in response to new information, sensory stimulation, development, damage, or dysfunction. In fact, for many years, it was considered dogma in the neurosciences that certain functions were hard-wired in specific, localized regions of the brain and that any incidents of brain change or recovery were mere exceptions to the rule, the concept of “Brain cannot Change”. However, since the 1970s and ’80s, neuroplasticity has gained wide acceptance throughout the scientific community as a complex, multifaceted, fundamental property of the brain. “Brain can Change” by two basic concepts in neuroplasticity: Compensation, recruitment of additional brain areas to perform a function and Reorganization, displacement of a primary brain area performing a specific function. Remodeling of neural circuits through plasticity can occur spontaneously or triggered by intensive training (e.g., experience-dependent plasticity) and biological treatments (Pharmacological agents and Transcranial Magnetic and Direct Current Stimulation).
There are four different types of neuroplasticity: map expansion, homologous area adaptation, Compensatory masquerade and Cross-modal reassignment
Map expansion, the first type of neuroplasticity, entails the flexibility of local brain regions that are dedicated to performing one type of function or storing a particular form of information. The arrangement of these local regions in the cerebral cortex is referred to as a “map.” When one function is carried out frequently enough through repeated behaviour or stimulus, the region of the cortical map dedicated to this function grows and shrinks as an individual “exercises” this function. This phenomenon usually takes place during the learning and practicing of a skill such as playing a musical instrument or in task specific training in stroke patients to improve specific function like arm or leg movements, speech, language, cognitive or swallow function. This is the most commonly used approach in neurorehab and utilize task specific training in improving function and I can remember many of my stroke patients, young and old regaining lost abilities with this approach.
Homologous area adaptation occurs during the early critical period of development. If a particular brain module becomes damaged in early life, its normal operations have the ability to shift to brain areas that do not include the affected module. The function is often shifted to a module in the matching, or homologous, area of the opposite brain hemisphere. This concept can help to improve speech and language function after stroke with involvement of dominant lobe. Where in the right brain in right hand dominant person is not involved in speech and language function, can take over function with repeated task specific training. Many of our stroke patients has shown significant improvement from global aphasia to motor aphasia and spontaneous speech production with long term supervised speech language therapy along with pharmacotherapy.
Compensatory masquerade, can simply be described as the brain figuring out an alternative strategy for carrying out a task when the initial strategy cannot be followed due to impairment. One example is when a person attempts to navigate from one location to another. Most people, to a greater or lesser extent, have an intuitive sense of direction and distance that they employ for navigation. However, a person who suffers some form of brain injury or stroke and impaired spatial sense will resort to another strategy for spatial navigation, such as memorizing landmarks. The only change that occurs in the brain is a reorganization of preexisting neuronal networks. This is a simple and novel way by which stroke survivors who were not able to do a complex everyday day task can be trained to do it themselves.
Another form of neuroplasticity, cross-modal reassignment, entails the introduction of new inputs into a brain area deprived of its main inputs. A classic example of this is the ability of an adult who has been blind since birth to have touch, or somatosensory, input redirected to the visual cortex in the occipital lobe of the brain—specifically, in an area known as V1. Sighted people, however, do not display any V1 activity when presented with similar touch-oriented experiments. This occurs because neurons communicate with one another in the same abstract “language” of electrochemical impulses regardless of sensory modality. This strategy is useful to improve visual / auditory functions after stroke.
Most the recent rehabilitation approaches to improve sensory-motor recovery including rehab robotics, virtual reality, mirror training, constraint induced therapy, task specific training intensive locomotor training work on the principles of neuroplasticity. This hold true for improving most of the functions after stroke including cognitive, visual, behavioral, speech, language, swallow, movements, tone or sphincter functions. I have taken example of stroke for simplification but this hold true to most of the diseases of nervous system including traumatic brain injury, multiple sclerosis, early dementia and Parkinsons’s disease, hypoxic and hypoglycemic encephalopathy etc. The rehab process should start as soon as possible, when patient’s are medically stable in the acute stage and continues from intensive care to inpatient wards to day care to outpatient care to home care and then leading to community integration.
I have treated so many patients with massive strokes and brain injury who were thought to remain in vegetative state or bed bound for life are now living independently in the community, thanks to the neuroscience and rehabilitation to unmask this gift of god and to use it to help our stroke and brain injury survivors.

Dr Abhishek Srivastava, MBBS, MD, DNB, PhD
Neurorehabilitation Specialist, Director, Centre for Rehabilitation,
Kokilaben Hospital, Mumbai