
Ulcerative Colitis is an auto-immune condition. Read this article to understand the symptoms, causes, treatment and management of Ulcerative Colitis
What is Ulcerative Colitis
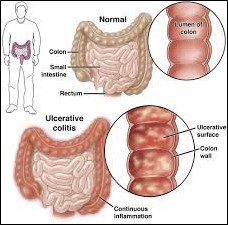
It is an inflammatory disease that usually begins in the rectum and may later involve the large intestine.
It is a lifelong autoimmune condition (the normal bowel bacteria provoke the immune system to attack the wall of the intestine, thus causing injury to the bowel).
It is a part of the spectrum of the inflammatory bowel disease in which inflammation causes injury and breakdown of the wall of the intestines.
It usually begins around the age of 30 but is known to occur until 60 as well.
Possible Causes and Triggers:
The exact cause is still unknown.
Sometimes, a viral or bacterial infection may activate the immune system in the intestine and it continues to stay active, thus causing inflammation even after the infection subsides.
Specific genes passed on from the parent may increase the risk of developing ulcerative colitis, with the right triggers like an infection.
Symptoms:
Usual symptoms are -
- Lower abdomen pain
- Loose stools containing blood and pus or mucus (the blood is usually from the rectum)
- Feeling of uneasiness before a bowel movement
- Increased urge for bowel movements waking one from sleep
- Cramps in abdomen
Other symptoms are -
- Loss of appetite
- Fever
- Fatigue
- Dehydration due to loss of fluids
- Weight loss
Tests needed to diagnose Ulcerative Colitis
Blood tests
They usually reveal signs of inflammation like a high white blood cell count.
Anemia (low hemoglobin) and an iron deficiency.
Liver function test may reveal inflammation of the liver ducts sometimes.
Stool tests
Used to detect infections that may be a possible cause of symptoms.
Flexible sigmoidoscopy or colonoscopy
A tube with a camera is inserted into the rectum, which allows visualization of the large intestine and is also used to get a biopsy (sample) from there.
Biopsy
During colonoscopy or sigmoidoscopy, the doctor takes a small sample of tissue from the wall of the intestine, which is then for signs of inflammation.
MRI
It is used to visualize the areas of ulcerative colitis involvement.
Treatment of Ulcerative Colitis:
Medications:
To prevent the inflammation of the intestines, for mild disease, steroids and/or anti-inflammatory drugs called amino salicylates (similar to aspirin) are prescribed by the doctors.
Immunomodulators to reduce and suppress inflammation and severe cases.
Antibiotics to prevent and treat infections.
Anti-diarrheal medication to control diarrhea and sometimes intravenous nutrition and fluids while the colon recovers.
Surgery:
After some surgeries, an opening is created in the abdominal wall called stoma, which is connected to a drainage bag.It helps to pass stools which replaces the function of the rectum.The stoma may be used temporarily or permanently.
The newer surgical techniques involve the removal of the lining of the rectum while preserving the muscular layer that helps the stools to be passed through the rectum.The stools are almost normal but may be more frequent and may contain more liquid.
Management of Ulcerative Colitis:
Since ulcerative colitis is a lifelong condition and has a waxing and waning course, the management involves mitigation of symptoms and associated food intolerance and nutritional deficiencies.
- Nutritional deficiencies:
Vitamin B12 deficiency is common in patients with Ulcerative colitis or intestinal surgeries.
Iron deficiency is also known to occur in patients with Ulcerative colitis.
Folate deficiency may be seen due to poor dietary intake or due to some medications used for treatment, like sulfasalazine, that may interrupt the folate metabolism.
Occasionally, ulcerative colitis may cause anemia that is unresponsive to replacement therapy (refractory anemia), it is managed by using synthetic erythropoietin.
Other micronutrient deficiencies to monitor and supplement for patients with ulcerative colitis may be magnesium, zinc and copper. - Vitamin D and calcium deficiency: Due to prolonged treatment with steroids, many patients may have weakened bones and may require supplementation of vitamin D and calcium.
- Protein calorie malnutrition:
In cases of severe colitis, there may be low protein and albumin levels in blood that are also indicators of severity and may require hospitalization and intravenous parenteral nutrition.
Patients with chronic severe malnutrition with massive resection of parts of the small intestine may need to be on home intravenous hyperalimentation therapy. - Low-fiber diet:
Low-fiber diet may help when the symptoms are active.
Prevention:
There is no prevention for ulcerative colitis, however, measures may be taken to prevent complications and severity.
- Prevention of symptoms: Knowing the family history and seeking early medical attention in case of changes in bowel habits like abdominal pain, diarrhea, weight loss or frequent vomiting may be helpful in early diagnosis and treatment and therefore preventing complications and severity.
- Regular heath checks may help in keeping the gut healthy and maintaining optimal gastrointestinal tract health.
- Dietary changes: Consuming a nutritious and -balanced diet low in fiber may be helpful in reducing any irritation to the inflamed intestinal wall of the intestines.Food to avoid may include alcohol, caffeine, beans, peas, and legumes, nuts, food items containing sorbitol like sugar-free gum, refined sugar and spicy food.
- Consuming probiotic rich food like yogurt, miso soup, etc.as they help to reduce overgrowth of bad bacteria in the gut.
- Regular exercise and de-stressing: Regular exercise and meditation help to maintain optimal health and also reduce stress, which is a trigger for Crohn’s disease.
REFERENCES:
- Crohn's & colitis foundation. “IBS vs IBD | Crohn’s & Colitis Foundation.” Crohn’s & Colitis Foundation, 2019, www.crohnscolitisfoundation.org/what-is-ibd/ibs-vs-ibd.
- “Inflammatory Bowel Disease or Irritable Bowel Syndrome? | Department of Surgery | Washington University in St. Louis.” Surgery.wustl.edu,surgery.wustl.edu/inflammatory-bowel-disease-or-irritable-bowel-syndrome/.
- “Diet and Nutrition.” Crohn’s & Colitis Foundation, www.crohnscolitisfoundation.org/diet-and-nutrition?trackBlock=true&….
- “Ulcerative Colitis.” Harvard Health, 1 Nov. 2020, www.health.harvard.edu/a_to_z/ulcerative-colitis-a-to-z.
- Harvard Health Publishing. “Crohn’s Disease - Harvard Health.” Harvard Health, Harvard Health, 15 Nov. 2018,www.health.harvard.edu/a_to_z/crohns-disease-a-to-z.
- Botoman, V. Alin, et al. “Management of Inflammatory Bowel Disease.” American Family Physician, vol. 57, no. 1, 1 Jan. 1998, pp. 57–68,
www.aafp.org/pubs/afp/issues/1998/0101/p57.html. - “Inflammatory Bowel Disease Treatment & Management: Approach Considerations, Symptomatic Therapy/Supportive Care, Overview of
Therapy.” EMedicine, 14 June 2021, emedicine.medscape.com/article/179037-
treatment?form=fpf&scode=msp&st=fpf&socialSite=google&icd=login_success_gg_match_fpf&isSocialFTC=true#d21. Accessed 12 Dec. 2023. - Mayo Clinic. “Ulcerative Colitis.” Mayo Clinic, 16 Sept. 2022, www.mayoclinic.org/diseases-conditions/ulcerative-colitis/symptoms-caus…-
20353326. - “Ulcerative Colitis.” AGA GI Patient Center, 13 July 2021, patient.gastro.org/ulcerative-colitis/.
















