
Medical emergencies work on their own timeline. They do not discriminate and when the time comes, time is of essence. Here are the top 7 emergencies everyone should know about and what you should do immediately.
HEART ATTACK
One of the most life threatening and commonly encountered emergencies is heart attacks or in medical terms Myocardial Infarction (MI). Immediate action can change the outcome and save lives.
What to expect:
A heart attack occurs when the plaque mostly made of fat formed inside the walls of the blood vessels obstructs the blood flow. Prolonged interruption of blood flow causes damage to the heart muscles and stops it from beating properly.
Must Read: How to be prepared for a medical emergency at home
Symptoms
- Pressure, tightness, or a squeezing sensation in the chest
- Pain may radiate from chest to the upper jaw or left shoulder or the arm
- There may be blackouts/fainting
- Excessive sweating
- Sometimes there may be no symptoms at all, especially in people with diabetes.
- The symptoms may begin slowly, with mild pain and can happen while one is at rest or active.
What Should You Do?
- If the person is conscious, give him an aspirin (Do not use an aspirin if someone is already on a blood thinner as it may cause bleeding) and take him/her to the nearest hospital for an ECG to confirm the status. If the person is unconscious: Follow AVPU
- A – Alert. The person is fully awake (may not be oriented). The person will spontaneously open eyes, will respond to voice and will have bodily motor function.
- V- Responding to voice. The person makes some kind of response when you talk to him. It could be opening his eyes, responding to your questions or initiating a move. These responses could be a small sound, a moan, or a slight movement of a limb when prompted by the voice
- P – Responding to pain. Applying a pain stimulus, like rubbing the breastbone or squeezing the fingers, can elicit a response from the person. Someone who is partially conscious can react by using their voice, eyes, or body.
- U – Unresponsiveness/Unconsciousness. When the person does not give any eye, voice or motor response to voice or pain.
START CPR if the patient is unresponsive:
A. Airway :
Open the airway by using the head tilt and chin lift:
- Carefully tilt the head back
- Lift the chin to open the airway
B. Breathing:
- Assess if the person is breathing ( approx. 10 seconds): Look to see if chest is moving up and down. Listen for sounds of breathing at the person’s mouth. Feel for breath on your hand or cheek.
- If the person is unresponsive, has an open airway, and is breathing, turn the person onto his side with the person’s hand in front. This will prevent choking if the person vomits.
- If the airway is blocked, clear the airway: Reposition with head tilt and chin lift. Check inside the mouth for an obstruction. Clear the airway with your finger
- Continue to check for breathing: Look, Listen and Feel
- Monitor until help arrives or until you can transport the patient to further care
- Continue to check for breathing by looking at the chest for rise and fall, feel with your hand in front of the mouth and nose and listen for breathing sounds.
C. Circulation: Start CPR (Cardio-pulmonary resuscitation) if they’re still not breathing
Chest compressions:
- Place the person on their back and kneel down beside them.
- Place the heel of your hand on the lower half of the breastbone, in the center of the chest. Place your other hand on top of the first hand and interlock the fingers.
- Position yourself directly above the patient’s chest.
- Use your body weight and keep your arms straight, press straight down on their chest. The release.
- One press down and release is 1 compression.
Mouth to Mouth Respiration:
- Open the person’s airway by placing one hand on the forehead and the other hand under the chin to tilt the head back.
- Pinch the nose so that it’s closed with your index finger and thumb.
- Open the person’s mouth.
- Take a breath and place your lips over the patient's mouth, making sure its sealed.
- Blow into their mouth for about 1 second while watching for the chest to rise.
- Following the breath, observe for the patient’s chest to fall. Listen and feel for signs that air is being expelled. Maintain the head tilt and chin lift position.
- Check the mouth again and remove any obstructions if the chest is not rising. Check that yours and the person’s mouth are sealed together and the nostrils are closed so that air cannot escape.
- Repeat the process
Give 30 chest compressions followed by 2 breaths, Ratio “30:2”.
Aim for 5 sets of 30:2 in about 2 minutes
If only the chest compressions are done, then about 100 – 120 compressions/minute.
Keep going with 30 compressions then 2 breaths until: the person recovers OR the ambulance arrives
When should CPR not be done?
- Obvious signs of Death
- Person is breathing normally
- On Arrival of the ambulance
- Unsafe area or hazardous situation e.g car accident on a busy road
CARDIAC ARREST
What to Expect:
A cardiac arrest occurs when a person’s heart stops pumping blood to their body and they stop breathing normally. Many cardiac arrests happen because of a heart attack. When the pumping action of the heart becomes irregular or stops, the heart may stop pumping blood to all vital organs like the kidneys, brain, lungs etc. and that can lead to loss of consciousness and death.
Symptoms:
- Sudden loss of consciousness
- No pulse
- No breathing
- Other preceding symptoms may be that of a heart attack
What should you do?
START CPR if the patient is unresponsive. To know more, read https://www.patientsengage.com/conditions/first-aid-cardiac-arrest
STROKE
What to expect:
Stroke happens when blood flow to an area of brain is cut off causing oxygen deprivation and death of those brain cells. As a result, the abilities controlled by that area of the brain such as memory and muscle control are lost. It not treated on time; it can cause long term complications like paralysis, loss of bowel and bladder control, pain in hands and feet.
Symptoms:
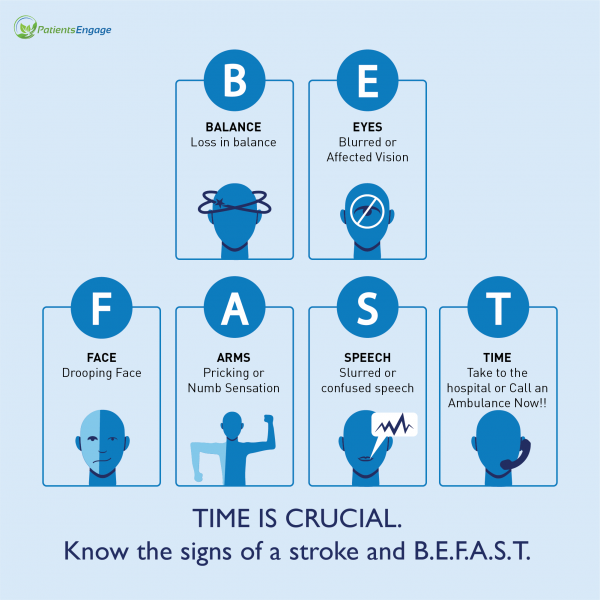
Stroke should be treated within treated 3 hours of the symptoms first appearing. If you suspect that someone may be having a stroke use the B.E.F.A.S.T test.
- Balance- Can the person walk? Is there dizziness or lack of coordination?
- Eye – Vision problems in one or both eyes like blurred vision.
- Face – Check their face. Does it seem asymmetrical?
- Arms – Can they raise both arms and keep them there?
- Speech – Is their speech slurred?
- Time is critical. If you notice any of these signs, call the nearby hospital
What should you do?
Conscious person
- Make the person sit/lie in a comfortable position.
- Call for an ambulance or rush the person to hospital.
Unconscious person
- Make the person lie on his/her left side (recovery position) with head and shoulders supported.
- Loosen any tight clothing around his/her neck and calm the patient.
- Try to maintain breathing, if needed with open mouth.
- Do NOT make the person eat or drink anything.
- Call for an ambulance or rush the person to hospital immediately.
FIT OR SEIZURE
What to expect:
Fits and seizures may happen in people who have a diagnosis of epilepsy or in other people too.
Symptoms:
- It may cause involuntary and uncontrollable jerking, twitching or shaking of part or entire body.
- Another form of fit or seizure can involve no movement or minimal movement of the body, and a person can appear to be looking into space. In this situation, a person will tend not respond when spoken to.
What should you do?
- Ease the person onto the floor.
- Turn the person onto their side to help them to breathe.
- Remove anything hard or sharp from around the person to prevent injury.
- Put something soft and flat, like a folded cloth, under his or her head.
- Remove eyeglasses.
- Loosen clothing or anything around the neck.
- Call for an ambulance if the seizure lasts longer than 5 minutes.
A consultation with a neurologist is always suggested following a seizure even if it lasted less than 5 mins.
FALLS
What to expect?
Falls occur more often with advancing age. Each year, approximately 26-37% of people aged 65 years and older who live in the community fall. Older adults with walk difficulty had a significantly higher likelihood of reporting fall-related injuries in comparison to others. Fall-related injuries cause discomfort and disability for older adults as well as stress for caregivers.
Common causes:
- Loss of balance
- Improper gait
- Dizziness due to medications or other causes like low blood sugar, sudden fall in blood pressure
- Slipping in the washroom
- Poor vision
- Arthritis- which may lead to joint stiffness and mobility issues
- Blood pressure fluctuation causing loss of consciousness or blackouts
Risks associated with falls in elderly:
- Fracture of bones. The hip, thigh and skull fracture can be very dangerous.
- Bruising
- Loss of consciousness due to concussion or brain bleed
- Mental trauma and anxiety
- Cuts and other wounds
What should you do?
- If you can call for help call out and avoid moving on your own if you feel pain on movement.
- Caregiver should wait until the shock wears off before moving the injured elderly
- If you suspect a fracture or the person complains of head or neck pain avoid moving them- Call for an ambulance
- If the person is unconscious, it may be a head injury, call for an ambulance and mobilize to a hospital for an examination
Always see a doctor for an assessment if you are unsure of the symptoms to ensure an assessment.
Things to do to avoid falls in elderly:
- Remove clutter and tripping hazards
- Install handrails for support in toilets and showers
- Ensure shoes have a good grip
- Have proper lighting at home
- Exercise to maintain core strength and balance
- Get enough sleep
- Avoid alcohol (Acceptable limit is up to one drink a day for women and up to two drinks a day for men; Examples of one drink include: Beer: 355ml,Wine: 148 ml, Distilled spirits 44ml.
How to prevent falls from the bed:
- Use a lower height bed
- Use a safety rail beside bed
- Gently roll over to the side and sit up and stay for few seconds and then get up using support
Related Reading: Preventing Falls Of Elderly At Home
BURNS
What to expect?
The common causes of burns:
- Thermal sources, including fire, hot liquids, steam and contact with hot surfaces, are the most common causes of burns.
- Chemicals like acids.
- Radiation burns.
- Electric burns
- Sun burns on skin.
Symptoms:
1st-degree burn.
- This is a minor burn and affects only the outer layer of the skin (epidermis).
- It may cause redness and pain.
2nd-degree burn.
- This affects both the epidermis and the second layer of skin (dermis).
- It may cause swelling and red, white or charred skin.
- Blisters may develop which may be very painful.
- Deep second-degree burns can cause scarring.
3rd-degree burn.
- This burn reaches to the fat layer beneath the skin.
- Burned areas may be black, brown or white.
- The skin may look leathery.
- Third-degree burns can destroy nerves, causing numbness.
What should you do?
First-degree burns:
- Run normal tap water over the burn area.
- Don’t apply ice. For sunburns you may apply aloe vera gel.
- For thermal burns, apply an antibiotic cream.
- Over-the-counter pain medication may be taken.
Second-degree burns: (needs a doctor’s assessment)
- Similar management to the first-degree burns.
- Your doctor may prescribe an antibiotic cream that contains silver, such as silver sulfadiazine to prevent bacterial infections.
- Elevate the burned area to reduce pain and swelling.
Third-degree burns: (needs a hospital visit)
- They can be life-threatening and often require skin grafts.
- Skin grafts replace damaged tissue with healthy skin from another of the uninjured part of the person’s body
CHOKING
What to expect?
Choking is when a person cannot breathe properly because something is blocking the airway.
Symptoms:
- Person suddenly holds his/her neck and gags
- Inability to talk, cry or make any sound
- Difficulty breathing
- Inability to cough
- Lips and tongue turn blue
- Loss of consciousness if blockage is not cleared
What should you do?
- If the person can speak, cough or breathe the encourage them to cough as a strong cough may often dislodge objects. If the person cannot speak, cough or breathe, follow the 5 and 5 approach: Give up to 5 back blows between the person’s shoulder blade with the heel of your hand. Check to see if the object is dislodged after every back blow.
- If the object is not dislodged: Perform the Heimlich Maneuver (see image)
- Stand behind the person and put your arms around their abdomen.
- Make a fist with one hand and clasp your other hand tightly around it.
- Place the thumb side of your fist just below their ribcage and about two inches above their navel.
- Sharply and quickly thrust your hands inward and upward five times.
- Repeat this process until the object is freed (dislodged) or the person becomes unconscious. If the person becomes unconscious, start CPR.

Related Reading: How to prepare for a medical emergency at home
References:
https://www.cdc.gov/epilepsy/about/first-aid.htm
https://www.ambulanceoncall.com/blogs/first-aid-common-medical-emergenc…
https://www.firstresponse.org.uk/.well-known/sgcaptcha/?r=%2Ffirst-aid-…
https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-1…" https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-022-1…
https://www.mdpi.com/2308-3417/8/2/43













