With growing occurrences of neurological disorders, an increased collaboration between neurology and palliative care or neuropalliative care services has become imperative, stresses Dr.Kaustubh Mahajan, neurologist at Hinduja Hospital, Khar. Also an extract from a paper presented by neurologist Dr Roopkumar Gursahani.
What is the role of palliative care in patients with neurological diseases?
There's a definite and very important role of palliative care in neurological diseases. There are so many patients with neurological conditions who have persistent disabilities that can't be treated to cure but can be managed by palliative care to keep patient and his family comfortable significantly.Our goal as a physician is not just to treat the disease but the patient as a whole and ensure he's comfortable as well.
Neurological diseases have been found to be the second most common condition, after oncological diseases, in patients seen by a palliative care. Why is it so?
There many cancers which can't be treated either because they're very aggressive and we don't have any treatment or because the cancer was identified late especially when it has already spread where treatment usually fails. Similarly, in neurology which involves brain and spinal cord, both being specialised organs, complete cure may not be possible in mostly degenerative and genetic conditions.
Do neurology patients such as those with Parkinson disease, dementia, multiple sclerosis, brain tumours, stroke, etc have unique palliative care needs?
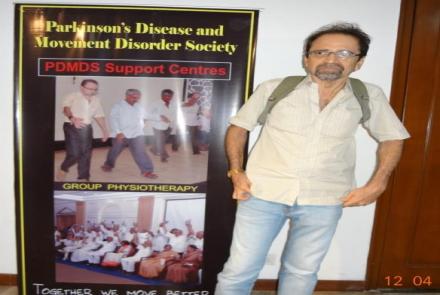
Yes, different neurological conditions have different palliative needs. For instance, degenerative neuro conditions like Alzheimer's, Parkinson's keep progressing and caretaker burnout also needs to be addressed. Patients with Stroke, infact, may slowly get better. Medications for these conditions may have side effects which must be known and tolerated at times. Patients with Multiple Sclerosis may feel drained because of depression as well which needs to be addressed and treated.
Palliative care in chronic, progressive, and incurable neurological conditions is being recognized now, though not widely practiced. Is there is still a wide range of unmet palliative care needs for neurology in India?
Yes, there are many other unmet palliative care needs to be still addressed in our country. Like critical patients in ICU with multiple organ dysfunction, with irreversible brain injury - sometimes rather than radical aggressive medical interventions, palliative approach would be preferable and financially helpful. Also, how to communicate to relatives and patients about their conditions who have or existing notion that nothing can be done - right communication is first step in palliative care.
With growing occurrences of neurological disorders and symptoms, do you think an increased collaboration between neurology and palliative care or neuropalliative care services has become imperative?
Yes, it has become imperative to collaborate neuro and palliative care, because as life expectancy is increasing with better conditions, more and more neurological conditions which need palliation are seen.
How can palliative care be integrated into neurology practice?
Palliative care needs to be and can be integrated with neurological practice. Infact, in some conditions palliative care plays more important role than just medical therapy. It starts with awareness amongst physicians about there's more to patients condition than just diagnosis and cure. During medical training itself this has to be taught. Medical students learn from their teachers or senior doctors.
What are the complexities and challenges of neuropalliative care services?
There are many complexities and challenges in neuropalliative care. Awareness is very less about palliative care among physicians as well as patients.Also palliative is a slow process with no immediate results like in curative treatments so satisfaction is also slow and gradual but definite. Also, there are not many palliative care centres. There should be more of them.
How can the delivery of neuropalliative care to patients be improved?
Delivery of neuro palliative care can be increased if we have more palliative care centres and home based therapy is provided.
Should home-based specialist treatment for severely affected neurological patients be advocated and promoted?
Yes,home based specialist treatment for severely affected neurological patients should be advocated and promoted.
What is the difference between palliative and end-of-life care?
There's a very thin line between both of them. One can tell where palliative care extends to end of life care.They're overlapping.
End-of-life care is an integral part of neurology practice, and neuropalliative medicine is an emerging neurology subspeciality. This begins with serious illness communication as a protocol-based process that depends on an evaluation of patient autonomy and accurate prognostication. Communication needs vary between chronic, life-limiting neurologic illnesses and acute brain injury. In an ideal situation, the patient's wishes are spelled out in advance care plans and living wills, and surrogates have only limited choices for implementation. Palliative care prepares for decline and death as an expected outcome and focuses on improving the quality of life for both the patients and their caregivers. In the Intensive Care Unit, this may require clarity on withholding and withdrawal of treatment. In all locations of care, the emphasis is on symptom control. Neurologists are the quintessential physicians, and our "dharma" is best served by empathetically bringing our technical knowledge and communication skills into easing this final transition for our patients and their families to the best of our ability.
(The above extract is taken from a paper on ‘Palliative care and the Indian Neurologist’by Dr Roopkumar Gursahani, Neurologist Consultant at Hinduja Hospital.
doi: 10.4103/0972-2327.192885 )