
Signs to watch for and how to prevent it. By family practitioner and paediatrician Dr Gita Mathai
What is childhood obesity?
Children older than two years and less than 19 years need to have their BMI (Body Mass Index) calculated when they visit their physician either for immunisation or during annual check-ups. BMI is calculated by dividing weight in kilograms by the height in meter squared.
You can also measure BMI at home. The values for height can be entered in the website below. It automatically provides the BMI.
https://nccd.cdc.gov/dnpabmi/Calculator.aspx
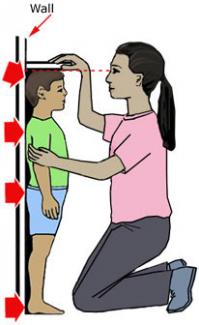
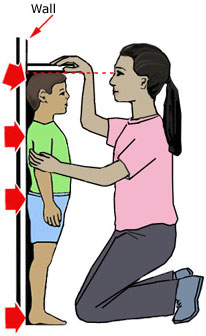
To measure a child’s height accurately at home, do the following. First remove the child's shoes, bulky clothing and hair ornaments. Spiked hair should be flattened.
- Take the height measurement against a flat surface, such as a wall.
- Have the child stand straight with feet flat and level shoulders.
- Make sure the child is looking straight ahead.
- Take the measurement while the child stands with head, shoulders, buttocks, and heels touching the flat surface (wall). (See illustration below).
- Use a flat headpiece to form a right angle with the wall and lower the headpiece until it firmly touches the crown of the head.
- Make sure the measurer's eyes are at the same level as the headpiece.
- Lightly mark where the bottom of the headpiece meets the wall. Then, use a metal tape to measure from the base on the floor to the marked measurement on the wall to get the height measurement.
- Accurately record the height to the nearest 1/8th inch or 0.1 centimeter.
To measure weight accurately at home:

1. Preferably use a digital scale. Place the scale on firm flooring.
2. Have the child or teen remove shoes and heavy clothing, such as sweaters.
3. Have the child or teen stand with both feet in the centre of the scale.
4. Record the weight to the nearest decimal fraction (for example, 55.5 pounds or 25.1 kilograms).
Check the growth chart (see link below) to see the percentile at which the child falls. The 85th percentile is the cut off for being “overweight”. The 95th percentile is the cut off for obesity. You can find the chart at the following link: http://www.cdc.gov/growthcharts/html_charts/bmiagerev.htm
How a child grows
Below the age of 2 years, weight gain depends on the birth weight. Children normally double the birth weight at the end of the 5th month and triple it at the end of the first year.
Children become active (they start to walk and run) after the first year. The weight gain in active children is only 2-3 kilos till the second birthday. After that the BMI charts should be used to keep tabs on development of obesity.
Another way to estimate obesity is to measure the skin fold thickness using skin calipers. The measurements are taken at the scapula and deltoid and then can be read off a graph.
https://www.health-calc.com/body-composition/skinfold-children
Can babies become overweight?
Yes, if you over-feed babies with breast milk or formula. Demand feeding (feeding the baby when it cries and stopping when it seems to have had enough) prevents this.
Babies have a built in appetite centre in the brain. They instinctively regulate their food intake. A child ideally should only triple its birth weight by the end of the first year.
Anxious parents and caregivers may miscalculate the amount they feel a child should have. Over feeding and force-feeding can result in obese infants.
What about weaning?
Weaning should ideally (as per World Health Organisation recommendations) start at the end of the 6th month or after 180 days. Avoid preservative-laden precooked ready-to-eat weaning foods with high sodium content. These promote obesity. Small quantities of home-cooked cereals, vegetables and mashed fruits are healthier.
When does childhood obesity set in?
Usually obesity can be diagnosed in children by the age of five years or when they start kindergarten. If a child is obese at age 5, and it is not tackled, they remain obese and carry that excess weight into adult life.
Why does childhood obesity occur?
Childhood obesity does not have a single cause. There are usually several factors all working together that result in the obesity.
- Diet is most important. High-fat calorie-dense foods laden with transfats are advertised in the media. Children often demand and receive these foods as snacks or as substitutes for meals. They are washed down with sugar-laden artificially flavoured juices or aerated cola beverages.
- The lifestyle is sedentary with many hours of television viewing, computer or video games. Children need a minimum of 20-30 minutes of aerobic activity a day. This is in addition to games in school. If the school does not have games, then 40-60 minutes of aerobic activity is essential.
- Obese children often come from obese families. Complex polymorphic genetic inheritance has been blamed but not proven. If the families are studied for generations, it is seen that there is steady overeating and very little physical activity.
- The modern lifestyle also contributes. Children seldom walk (it may be dangerous). They are chauffeured everywhere by parents or others.
- Rarely the obesity may be due to hormonal imbalances like hypothyroidism or Cushing’s disease. If the BMI calculated is above the 95th percentile, consult a doctor to rule out disease and get a diet and exercise plan (if the problem is obesity).
What are the complications of childhood obesity?
- The bones may be unable to support the weight. The femoral epiphysis may slip (a shift in the upper part of the thigh bone). Bow legs may develop.
- The lipid profile may become deranged with elevated cholesterol and triglycerides. This can get deposited in the liver, blood vessels, and gall bladder causing gall stones.
- They may develop high blood pressure.
- Breathing difficulties and snoring may occur.
- Oestrogen, progesterone and androgen levels may get deranged with early onset of menarche (first menstrual bleeding) and later menstrual irregularities.
- The blood sugars can be elevated and diabetes can develop.
- These children suffer from low self-esteem, may be depressed and may be victims of bullying in school.
How can parents help?
Good parenting is the key to the prevention of childhood obesity.
- Children cannot be given weight-loss medications. Nor is it advisable to perform surgery. The long-term effects of both on growing children are not yet known.
- Physical activity burns calories and is essential for weight loss. At least an hour of activity is required a day. It is important to lead by example. Active parents have active children.
- TV viewing should be reduced to an hour or two on weekends only.
- Computers are not really meant for games. Sitting fixed and immobile in front of the console will definitely pile on the kilos.
- The diet should consist of home cooked meals, not ready-to-eat fried items. There should be 4-6 helpings of fruit and vegetables a day. Snacks should preferably be fruits. Snacks should not be offered as a reward.