When you or a loved one is first diagnosed with cancer, there are a lot of new terms to deal with. There are also a lot of questions about how treatment delivery mechanisms. This article addresses these unanswered questions. You can also refer to the glossary for more information on cancer terminology.
If you or your loved one has been through cancer treatment, you may be aware of the various types of medical inserts used by Oncologist for Chemotherapy.
Most medicines are injected into the vein of a person so it directly goes to the heart; this is called intravenous or IV. To make IV easier, ports or catheters are often used. They may be used to drain fluids, take blood samples, give transfusions, antibiotics and/or deliver food to the body. In cancer, they are a suitable method because:
- They can be used to provide the chemotherapy and other drugs to the body periodically at the scheduled cycles.
- Eliminates the problems of frequent pricking which leads to bruising and scarring of the arms.
- Convenient in case of small or collapsed veins especially in patients with significant weight loss.
- Helpful in patients who have needle phobia.
- Prevents skin damage from drugs and leaking of drugs from a punctured small vein.
- Allows for patients to have chemotherapy at home via a continuous infusion pump.
- Once inserted can last for months and provides a semi-permanent access point for the medical team.
- Easily removed soon after treatment is completed.
Depending on the patient’s treatment plan, duration, cost and ability to take care of the medical device, the Oncologist may decide to use ports or catheters. A port is a plug-like device inserted under the skin to connect to a major vein. A catheter is a thin flexible plastic tube that goes into a major vein.
Here are the four types of ports and catheters used in Cancer therapy:
- IV Catheter is the IV line commonly used. It is inserted on the back of the hand and can stay for a few days.

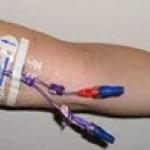
- PICC (peripherally inserted central catheter) is a line placed in the inner elbow and can stay for weeks to months.
- Central Line or Hickman catheter is also a long-term line placed under the collarbone. This too can last weeks to months.

- Implantable or Chemo port is an implant that goes under the skin and connect to a vein. The port can also keep for months.

How to care for your port or catheter?
Taking good care of your port or catheter is important and will be explained to you by your medical team. Common instructions are:
- Wash your hands before touching the catheter/port to prevent infections.
- Clean the insertion site and change the bandage as instructed
- The bandage covering the catheter insertion site should not become wet, so cover it with plastic before showering, going out in the rain or swimming. If you have a port, since it is already covered by skin, you are able to shower, swim etc without any fear of it becoming wet.
- If you have a port, you may be instructed on how to flush it.
- Never touch the open tip of the catheter when treatment is on.
- After treatment is finished, the catheter tip should be shut tight to avoid air from entering the tube.
|
Your medical team will have a conversation with you on what it is, what it does, and how to take care of it. If you do not get this information or have any questions or uncertainties, make sure you ask your doctor about it.
|
When to inform your doctor?
Although ports and catheters are routinely used in cancer treatment, they may cause certain side-effects in some patients. This includes infections, and blood clots or blockages. Always check the site in front of a mirror when cleaning it and changing the bandage. If you notice any of the following changes, report it to your doctor right away.
- Redness, swelling, bruising or pain at the site
- Leakage of any fluids
- Fever
- Difficulty breathing
- Changes in your heartrate
- Tube sliding out or twist in the tube
- Any blockage that prevents liquid from going in easily.
Your medical team will have a conversation with you on what it is, what it does, and how to take care of it. If you do not get this information or have any questions or uncertainties, make sure you ask your doctor about it.</td> </tr> </tbody> </table> <h3 class=">
|
Important tip:
Carry your port/catheter insertion medical document with you when travelling especially by air as it will be needed during security screening.
|
References:
Ports and catheters. Cancer Treatment Centers of America. (2021, September 21). Retrieved March 17, 2023, from https://www.cancercenter.com/treatment-options/ports-and-catheters
Catheters and ports in cancer treatment. Cancer.Net. (2021, February 10). Retrieved March 17, 2023, from https://www.cancer.net/navigating-cancer-care/how-cancer-treated/chemot…
















