One of the many unpleasant aspects of treatment for cancer patients is the adverse effect of having nerve related pain, tingling, altered sensations, etc. This is termed as neuropathy and occurs when the nerves fibers in the body get damaged, inflamed or destroyed during the cancer treatment process. Neuropathy can be managed with the help of physiotherapy and some lifestyle changes. Manali Kamat, a Physiotherapist from Tata Memorial Hospital, Mumbai provides detailed insight into this condition with easy tips for daily living.
What is neuropathy? Which types of neuropathies are seen in persons with Cancer?
There are 3 types of neuropathies predominantly seen:
- Sensory: Chemotherapy-induced peripheral neuropathy or CIPN is predominantly sensory. In sensory affection, patients complain of numbness, tingling, burning, and altered sensations in the hands and feet.
- Motor: Motor affection is less frequent than sensory. Patients usually find difficulty doing fine motor tasks such as buttoning, holding small things in hand, wearing footwear, walking etc.
- Mixed: Along with sensory and motor affection, sometimes the autonomic nervous system is also affected. If so, then patients may have irregular heartbeat, feel giddy after sitting up from lying down, and excess sweating in palms and feet.
Why do cancer patients get neuropathy?
There are multiple causes of neuropathy in cancer. The disease itself can cause neuropathy, by involving a nerve or compressing it. The side effect of treatment and co-morbidities like diabetes are some of the main causes.
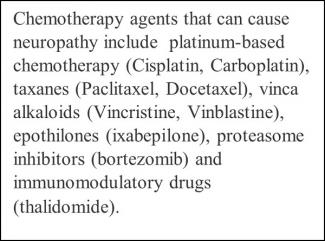
- Most of the cancers are treated by chemotherapy drugs. These drugs help to arrest the progression of cancer cells through different targets and mechanisms of action. But unfortunately, these drugs also act on normal cells and body structures. When these chemotherapy agents damage the nervous system and cause varying degrees of symptoms are called neuropathy or chemotherapy-induced peripheral neuropathy (CIPN). It depends on the different classes of drugs, their properties, and the dosage. The prevalence of CIPN varies between 19 to 85%. Either a single dose of chemotherapy or collective doses are major risk factors. The mechanism by which these chemotherapy drugs affect the nervous system is by damaging the nervous system structures, and the DNA or causing neuroinflammation. These chemotherapy agents (see box) produce varying degrees of neuropathy symptoms.
- Paraneoplastic effect- Our body produces antibodies against certain antigens (type of proteins) expressed by cancer, mostly seen in lung cancer. This phenomenon is called paraneoplastic encephalomyelitis. Patients are presented with progressive sensory neuropathic symptoms such as numbness, alteredsensations, and tingling in the hand. The picture is usually unilateral. Progressively patient may lose control of bodily movement (ataxia), awareness of the position of the body (body perception), confusion, memory loss, depression, and seizures.
- In certain cancers such as leukemia and lymphoma, cancer cells can enter into the nerves which results in mono-neuropathy (weakness of one limb), polyneuropathy (weakness in more than one limb), or plexopathy (network of nerves, blood vessels, or lymph vessels are affected).
- Certain non-cytotoxic medications such as antimicrobial agents, cardiovascular medications, and anti-convulsants can produce sensory-motor polyneuropathic symptoms.
- Patients with a history of diabetes can have neuropathy due to high blood sugar levels which injure nerves throughout the body. The most common presentations are either peripheral neuropathy, autonomic symptoms, or neuropathy where hip and thigh muscles are affected, and focal neuropathy where only one single nerve can be damaged.
- Bone marrow transplantation or BMT- Certain blood cancers such as leukemia may require a bone marrow transplantation. After the procedure, patients develop certain disorders resulting in polyneuropathies.
Are certain patients more at risk than others? How so?
Patients who receive certain types of chemotherapy (see box above) are susceptible to CIPN. It is important to consider the route of administration of chemotherapy. For example- bortezomib when given subcutaneously reduces the neuro- toxicity. Paclitaxel causes symptoms immediately after administration. CIPN symptoms usually develop after chemotherapy completion and the severity depends on the total dose. Some patients experience worsening of symptoms after completion of treatment. This phenomenon is called “coasting” where either mild neuropathy worsens or new CIPN develops.
Patients with a history of diabetes and bone marrow transplantation are at higher risk of developing neuropathy.
Can nerve damage be a sign of cancer or metastasis or is it always a side effect?
The nervous system can be involved in primary brain and spinal cord tumours. There is a direct invasion in nerves, its root, and even in muscles by the tumour itself. The patient develops symptoms such as sensory problems like pain and motor weakness in the limbs.
Brain metastasis can be a common site for many tumours. Metastasis is rare in nerves but few case studies are reported in the literature.
Most commonly, chemotherapy-related peripheral neuropathy is seen due to toxic effect of the chemotherapy drug.
How and who diagnoses neuropathy?
Clinicians or treating Oncologists diagnose neuropathy using different tools. Clinical examination and thorough patient history with signs and symptoms are recorded. The most commonly used objective evaluation is interference with activities of daily living such as slipping of chappals (open footwear) while walking, difficulty in buttoning the shirt, and other activities which involve small joints of hand and feet. The diagnosis of neuropathy should be approached with care as some patients may have co-morbid conditions such as diabetes which may also cause neuropathy. Such patients should be thoroughly evaluated for symptoms before starting chemotherapy.
The clinical symptoms are subjective and usually sensory. The diagnosis depends on the presence and severity of symptoms. If symptoms interfere with daily living, then the decision to discontinue chemotherapy may be made in extreme cases.
Patient assessments are done by treating physicians before starting chemotherapy, during cycles, and post-chemotherapy. The patient and the caretaker should be educated on the symptoms of CIPN so that if the patient develops any signs, it should be immediately reported to the Physician.
What signs and symptoms should a patient look out for?
Initial symptoms are usually sensory and the picture is bilateral.
- Sensory symptoms usually develop first in the feet and hands. This is also termed glove and stocking neuropathy where small joints of hands and feet show symptoms such as numbness, tingling, and altered or abnormal touch sensations.
- Some patients may experience painful sensations such as burning, shooting, or shock-like pain.
- Some may manifest allodynia (pain due to a stimulus that does not elicit pain) and hyperalgesia (increased pain from the stimulus which produces pain).
- In severe cases, the patient may lose sensory perception.
- Patients may have small joint weakness, gait, and balance disturbances. These symptoms affect the quality of life and safety.
- In severe cases, CIPN can lead to paresis or severe weakness of affected body parts, complete immobilization, and severe disability.
- Autonomic symptoms usually involve constipation, altered sexual function, trouble urinating, irregular heartbeat, drop in BP on standing up, and changes in sweating (sweating too much or too little).
When should a patient see a Physiotherapist? How does Physical therapy help?
Neuropathy symptoms result in functional difficulties which affect day-to-day work such as domestic, recreational, and social responsibilities. Some patients develop balance and movement difficulties which increase the risk of falls. Physiotherapists help in assessing and managing these symptoms and thus improve the quality of life.
Recent advances suggest that engaging in some kind of physical activity helps patients to improve their symptoms. There are various types and modes of exercises that can be planned according to the difficulties faced by the patient. Along with the exercise program patients should be educated about self-monitoring, discussing the symptoms at each follow-up, self-care, education to the caregiver, and taking help of others if needed.
Is there a way to measure neuropathy?
There are different grading systems used for CIPN. The most commonly used system is developed by the World health organization (WHO). It is a numerical system grading scale:
| Grade 0 | no symptoms |
| Grade 1 | paraesthesia (abnormal sensations) and/or decreased tendon reflex |
| Grade 2 | severe paraesthesia and/or mild weakness |
| Grade 3 | intolerable paraesthesia and/or marked motor loss (severe weakness) |
| Grade 4 | paralysis |
Along with the grading system, patient-reported outcome measures are used to compare the difficulties faced by patients in day-to-day activities.
What exercises are recommended for neuropathy?
Usually, exercise sessions are based on endurance training, strength training, balance, coordination, and flexibility exercises. These exercises can be done by using free weights, dumbbells, TheraBand, stationary bicycles, and exercise mats. A set exercise program can be done either via a supervised or a home-based program, and the patients have to be assessed periodically so that intervention can be modified according to need.
How can patients manage their neuropathy? Self-care Tips for daily living.
As symptoms of neuropathy are usually sensory patients have to be careful while doing household activities and activities for self-care. Sensory symptoms usually affect hands and feet where the patient feels numbness, burning, and tingling sensations. To protect oneself from any injury certain tips are mentioned below:
- Use rubber gloves while doing household work like cooking, cutting, washing utensils etc.
- Be cautious with sharp objects such as a knives, needles, forks, gardening or DIY tools.
- Use well-padded pot holders when cooking.
- Examine fingers and feet at least once a week for cuts and scratches.
- In cold weather, cover hands and feet with gloves and socks.
- Wear closed-toes shoes when going out.
- Avoid driving or riding a vehicle if you have altered sensations.
- Avoid walking on uneven surfaces.
- Use handrails while climbing and for toilet activities.
- Use support such as a cane or walker if needed.
- Use night lamps while sleeping.
Patients can follow certain food habits:
- Avoid sweets and sugary foods to maintain blood glucose levels.
- Include foods that are high in Vit B12 such as milk, egg, meat, and fish.
- Limit or avoid alcohol.
- Eat whole grains.
Can neuropathy be reversed?
Symptoms of neuropathy may usually decrease after discontinuation of chemotherapy. Some drugs develop new symptoms after months or years after treatment while some drugs cause permanent damage and symptoms will be present for a lifetime. Approximately 50-90% of patients experience neuropathy during the treatment. Many neuropathic symptoms can be reversed after dose reduction or discontinuation of therapy. Certain medications are used to prevent side effects of chemotherapy treatment. Studies have proven that after initiation of chemotherapy, regular functional exercises such as mobility, and sensory-motor training help to reduce the symptoms and prevent functional impairments.
How long do patients have to continue Physiotherapy? Can physiotherapy be stopped after improvement?
According to symptoms exercises should be continued till completion of treatment. If symptoms improve after cancer treatment completion one should engage in regular physical activity.
References:
- Neuropathy in the Cancer Patient: Causes and Cures.Sasu-Tenkoramaa J, Fudin J. Pract Pain Manag. 2013; 13(3).)
- Chemotherapy-Induced Peripheral Neuropathy: Current Status and Progress, Jamie R Brewer, Gladys Morrison, et al,Gynecol Oncol. 2016 January; 140(1): 176–183. doi:10.1016/j.ygyno.2015.11.011.
- Diagnosis, Management, and Evaluation ofChemotherapy-Induced Peripheral Neuropathy, Frederick H. Hausheer, Richard L. Schilsky, Semin Oncol 33:15-49, doi:10.1053/j.seminoncol.2005.12.010
- Chemotherapy-induced peripheral neuropathy (Review),Xia Zhang, Wei-Wei Chan and Wen Juan Huang,Biomedical Reports, 6: 267-271, 2017,DOI: 10.3892/br.2017.851
- Mechanisms of Chemotherapy-Induced Peripheral Neuropathy,RenataZaja˛czkowska, Magdalena Kocot-Ke˛pska, Int. J. Mol. Sci. 2019, 20, 1451; doi:10.3390/ijms20061451
- Neurologic Complications of Cancer and its Treatment, Pierre Giglio and Mark R. Gilbert, Curr Oncol Rep. 2010 January; 12(1): 50–59. Doi: 10.1007/s11912-009-0071-x.
- Grading of chemotherapy-induced peripheral neuropathy. J. Postma & J. J. Heimans, Annals of Oncology 11: 509-513. 2000.
- Non-Pharmacological Self-Management Strategies for Chemotherapy-Induced Peripheral Neuropathy in People withAdvanced Cancer: A Systematic Review and Meta-Analysis. Megan Crichton, Patsy M. Yates, Nutrients 2022, 14, 2403. https://doi.org/10.3390/nu14122403
- A systematic review of behavioural and exercise interventions for the prevention and management of chemotherapy-induced peripheral neuropathy symptoms, Mary Anne Lagmay Tanay, Jo Armes et al, Journal of Cancer Survivorship (2023) 17:254–277, https://doi.org/10.1007/s11764-021-00997-w