Stroke rehabilitation is an important aspect of the management of stroke. It can help to maximize recovery and regain as much of the body functions that is lost after a stroke, emphasises G Srinithya, Senior Occupational Therapist at NIMHANS.
What is Post Stroke Rehabilitation?
Post stroke Rehabilitation is a patient-centred, goal driven process that attempts to maximise the functional independence of patients who suffer from variety of stroke related disabilities. The aim of rehabilitation is to assist the stroke survivor to return to their premorbid functioning (or as close to it as possible) within their family environment, community environment, and where possible, work environment. Rehabilitation also teaches survivors new ways of performing tasks to circumvent or compensate for any residual disabilities.
What is the best time to restart rehabilitation in stroke survivors?
Rehabilitative therapy begins in the acute care hospital after the person’s overall condition has been stabilized, often within 24 to 48 hours after the stroke. The first steps involve promoting independent movement because many individuals are paralyzed or seriously weakened.
Patients are prompted to change positions frequently while lying in bed and to engage in passive or active range of motion exercises to strengthen their stroke impaired limbs. Depending on many factors - including the extent of the initial injury - patients may progress from sitting up and being moved between the bed and a chair to standing, bearing their own weight, and walking, with or without assistance. For some stroke survivors, rehabilitation will be an ongoing process to maintain and refine skills and could involve working with specialists for months or years after the stroke.
Which are common impairments that can result from a Stroke?
The disabling effects of a stroke are dependent on the affected areas of the brain. It is difficult to compare one individual’s disability to another, since every stroke can damage slightly different parts and amounts of the brain.
Generally, stroke can cause five types of disabilities:
- Paralysis or problems controlling movement
- Sensory disturbances including pain
- Problems with thinking and memory
- Emotional disturbances
- Problems using or understanding language
1) Paralysis or problems controlling movement
The paralysis is usually on the opposite side from where the brain is damaged by stroke, and may affect the face, an arm, a leg, or the entire side of the body. This one-sided paralysis is called hemiplegia if it involves complete inability to move or hemiparesis if it is less than total weakness. Stroke patients with hemiparesis or hemiplegia may have difficulty with everyday activities such as walking or grasping objects. Some stroke patients have problems with swallowing, called dysphagia, due to damage to the part of the brain that controls the muscles for swallowing. Damage to a lower part of the brain, the cerebellum, can affect the body’s ability to coordinate movement—a disability called ataxia—leading to problems with body posture, walking, and balance.
2) Sensory disturbances including pain
Stroke patients may lose the ability to feel touch, pain, temperature, or position. Sensory deficits also may hinder the ability to recognize objects that patients are holding and can even be severe enough to cause loss of recognition of one’s own limb. Some stroke patients experience pain, numbness, or odd sensations of tingling or prickling in paralyzed or weakened limbs—a symptom known as paraesthesia. A stroke patient’s decreased mobility also puts them at high risk for deep vein thrombosis and pulmonary embolism.
3) Problems with thinking and memory
Stroke can cause damage to parts of the brain responsible for memory, learning, and awareness. Individuals also may lose their ability to make plans, comprehend meaning, learn new tasks, or engage in other complex mental activities. Two fairly common deficits resulting from stroke are anosognosia, an inability to acknowledge the reality of the physical impairments resulting from stroke, and neglect, the loss of the ability to respond to objects or sensory stimuli located on the stroke-impaired side. Stroke survivors who develop apraxia (loss of ability to carry out a learned purposeful movement) cannot plan the steps involved in a complex task and act on them in the proper sequence.
4) Emotional disturbances
Many people who survive a stroke feel fear, anxiety, frustration, anger, sadness, and a sense of grief for their physical and mental losses. Clinical depression, which is a sense of hopelessness that disrupts an individual’s ability to function, appears to be the emotional disorder most commonly experienced by stroke survivors. Signs of clinical depression include sleep disturbances, a radical change in eating patterns that may lead to sudden weight loss or gain, lethargy, social withdrawal, irritability, fatigue, self-loathing, and suicidal thoughts. Post-stroke depression can be treated with antidepressant medications and psychological counselling.
5) Problems using or understanding language (aphasia)
A stroke-induced injury to any of the brain’s language-control centres can severely impair verbal communication. The dominant centres for language are in the left side of the brain for right-handed individuals and many left-handers as well. Damage to a language centre located on the dominant side of the brain, known as Broca’s area, causes expressive aphasia. People with this type of aphasia have difficulty conveying their thoughts through words or writing. They lose the ability to speak the words they are thinking and to put words together incoherent, grammatically correct sentences. In contrast, damage to a language centre located in a rear portion of the brain, called Wernicke’s area, results in receptive aphasia. People with this condition have difficulty understanding spoken or written language and often have incoherent speech. Although they can form grammatically correct sentences, their utterances are often devoid of meaning. The most severe form of aphasia, global aphasia, is caused by extensive damage to several areas of the brain involved in language function. People with global aphasia lose nearly all their linguistic abilities; they cannot understand language or use it to convey thought.
What medical professionals specialize in post-stroke rehabilitation?
- Physical Medicine Rehabilitation Specialist ( PMR )
- Rehabilitation nurses
- Physical therapists
- Occupational therapists
- Speech-language pathologists
- Psychologist
- Social workers
Physicians
Physicians have the primary responsibility for managing and coordinating the long-term care of stroke survivors, including recommending which rehabilitation programs will best address individual needs. Physiatrists are medical doctors who specialize in physical medicine and rehabilitation including pain management and spine problems. They help people regain function after surgery, a stroke, or an injury. They lead the team of health professionals mentioned below.
Rehabilitation Nurse
Nurses have been described as key players in interdisciplinary in‐patient stroke rehabilitation teams. Being present 24/7, they have unique opportunities to influence inpatient stroke re‐rehabilitation.
Physiotherapy
Physical therapists specialize in treating disabilities related to motor and sensory impairments. They are trained in all aspects of anatomy and physiology related to normal function, with an emphasis on movement. They assess the stroke survivor’s strength, endurance, range of motion, gait abnormalities, and sensory deficits to design individualized rehabilitation programs aimed at regaining control over motor functions. The physical therapy emphasizes practicing isolated movements, repeatedly changing from one kind of movement to another, and rehearsing complex movements that require a great deal of coordination and balance, such as walking up or down stairs or moving safely between obstacles. The stroke survivors tend to avoid using impaired limbs, a behaviour called learned non-use. However, the repetitive use of impaired limbs encourages brain plasticity and help reduce disability.
Occupational Therapy
Occupational therapy practitioners collaborate with clients and their families or caregivers to determine what activities are necessary, meaningful, and/or relevant to them. Many stroke survivors have changes in their physical, cognitive, and emotional abilities that impede them from independently performing their daily activities related to work, school, parenting, or leisure. Depending on the extent of the stroke, the needs and goals of the client, and the phase of stoke recovery, occupational therapy goals and services may include, but are not limited to the following:
- Further retraining in self-care skills and adapting tasks or environments (post-rehab), including the appropriate use of adaptive equipment to maximize the ability to perform activities of daily living (ADLs) safely (e.g., bathing, dressing, functional mobility)
- Addressing ongoing deficits such as weakness, sensory loss, and cognitive or visual impairments that limit engagement in ADLs and instrumental ADLs (IADLS: carrying groceries, cooking a meal, managing money, parenting)
- Training in community reintegration and modifying tasks or environments, including, where appropriate, assessment of and training in the use of assistive technology, to maximize independent engagement in IADLs.
- Performing work-related task analysis and work site evaluations, and recommending modifications to the workplace; collaborating with educational facilities to facilitate return to school; working with the client on child-care-related tasks and adaptations for safe parenting responsibilities; and recommending adaptations to resume former leisure activities or develop new ones as feasible.
- Evaluating and treating swallowing difficulties
- Developing coping strategies to support psychosocial health and well-being (including relaxation techniques, if appropriate)
- Teaching and promoting healthy lifestyle habits and routines to minimize risk of secondary stroke
- Developing strategies to overcome barriers to sexual intimacy
- Providing pre-driving and driving evaluations, equipment recommendations for safe return to driving, or education on alternate means of transportation
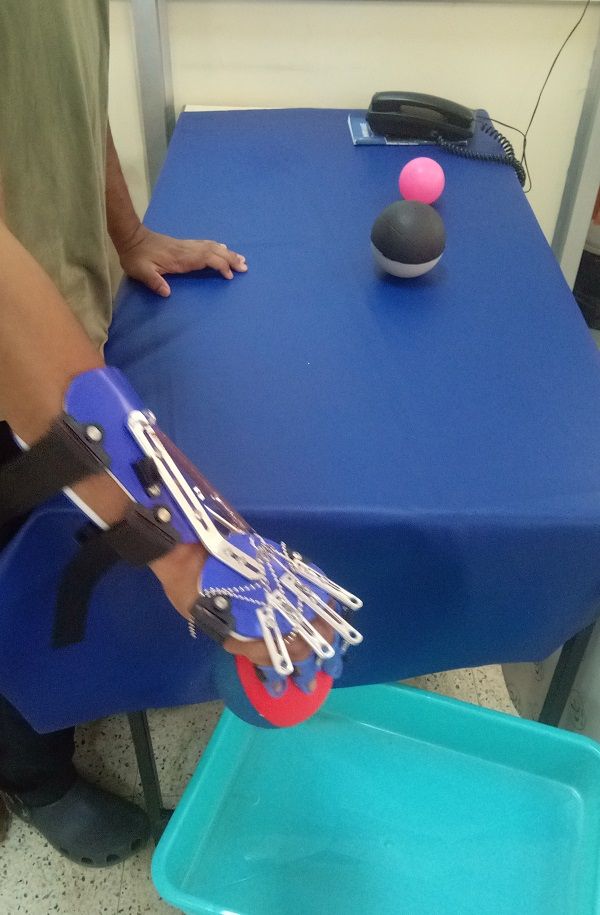
Prosthetists and orthotists
Prosthetists specialize in the fabrication of artificial limbs (prostheses) and orthotists specialize in fabricating devices (orthotics) to support or control a part of the body--such as an arm or leg--that has been impaired due to recent surgery, stroke, or injury. These devices include a range of splints, braces, and special footwear. The prosthetists and orthotists work alongside doctors, nurses, physical therapists, and occupational therapists to provide the best possible rehabilitation.
Speech-language pathologists
Difficulty in communication is one of the most serious complications of stroke. Over 33% of stroke patients have some form of speech, language and cognition issues immediately after stroke. Many recover within a few months, but 60% continue to have speech and language over 6 months post-stroke. For these people, or for people who struggle to communicate early on in their recovery, it is important to use various tools and techniques to augment their communication. In the process of recovery, these individuals show communication disorders in various forms.
An important part of the speech and language therapist’s role involves finding alternative or additional ways of communicating, which may include (a) gestures (b) writing (c) flash cards or (d) drawing. All assessments and interventions chosen must be culturally appropriate and endow with quantitative as well as qualitative information. For a healthy communicating environment is also very important for friends and family members to receive training on how to adapt their own communication style to allow for the person to participate in conversations and social activities.
Psychologist
When you realise what’s happened you are still scared, but now other emotions come into play; anger, sadness, depression, low self-esteem, just to mention a few. To be able to try to express your feelings to someone who appears to understand, is in my opinion vital to the recovery process.

G Srinithya, Senior Occupational Therapist at NIMHANS.